Evaluating the impact of kidney transplant timing on postoperative dialysis requirement and mortality in liver transplant patients: a single center experience
Daisuke Noguchi1, Jasmine Deng1, Vicky M Nguyen1, Jennifer Li1, Vatche G Agopian1, Samer Ebaid1, Douglas G Farmer1, Fady M Kaldas1.
1Liver and Pancreas Transplantation, Department of Surgery, David Geffen School of Medicine at UCLA, Los Angeles, CA, United States
Purpose: Renal insufficiency often occurs in patients with cirrhosis awaiting liver transplantation (LT). Although some of these patients require kidney transplantation (KT), guidelines on allocating kidney grafts for LT candidates continue to evolve. The aim of this study was to evaluate the outcomes of combined liver-kidney transplantation, compared with LT alone, and develop a new risk index for dialysis requirement at 12-month-post-LT (12M-pLT).
Methods: Adult LT recipients at our institution between January 2017 and December 2020 were retrospectively reviewed. Patients receiving LT for malignant tumors were excluded. LT patients were divided into two groups, simultaneous liver-kidney transplant (SLKT) and no SLKT. The no SLKT group was further divided into LT alone (LTa) and KT after LT (L-K). Dialysis requirement at 12M-pLT was assessed across all groups. Survival and multivariate analyses were performed to identify risk factors for dialysis at 12M-pLT.
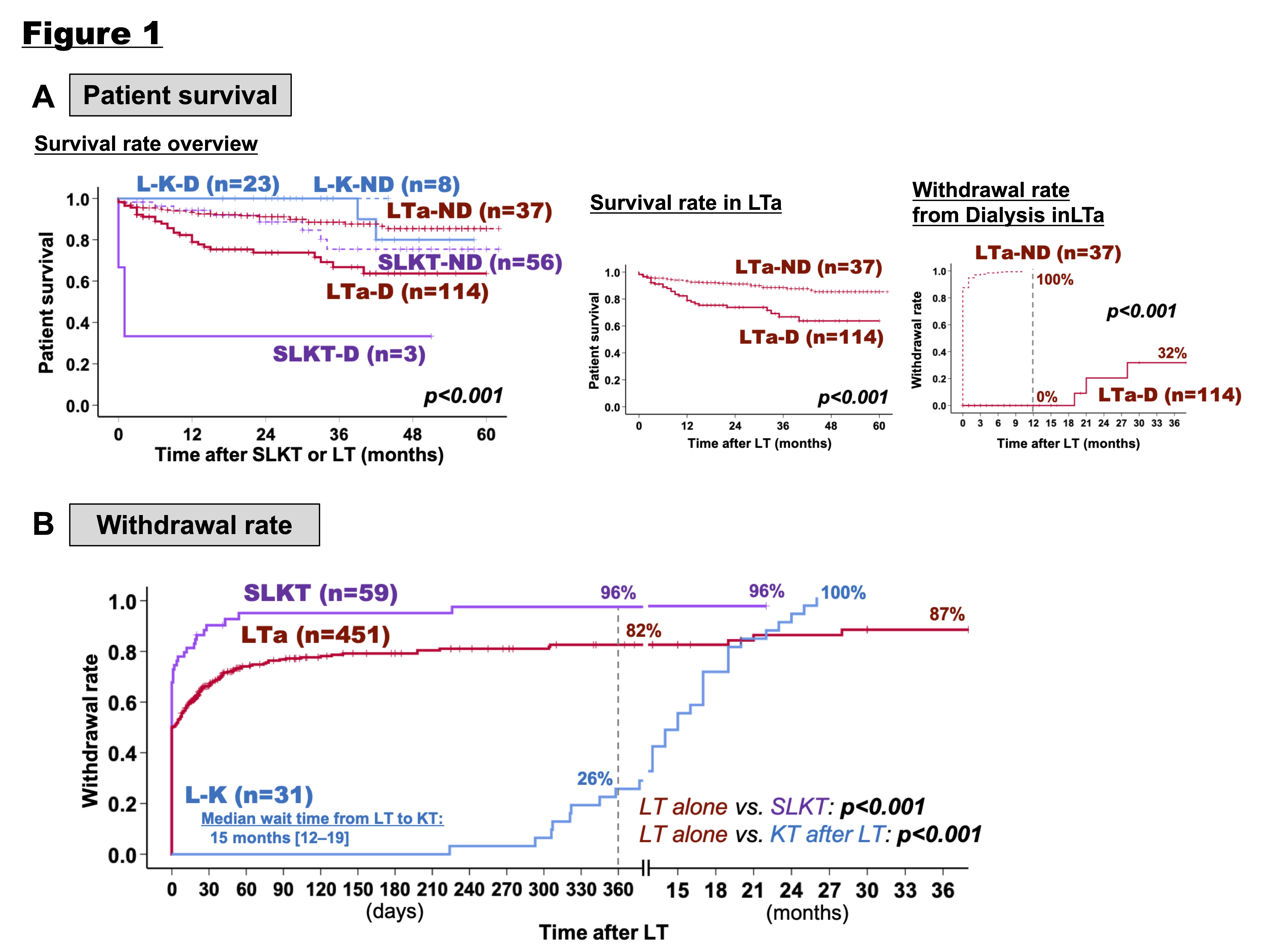
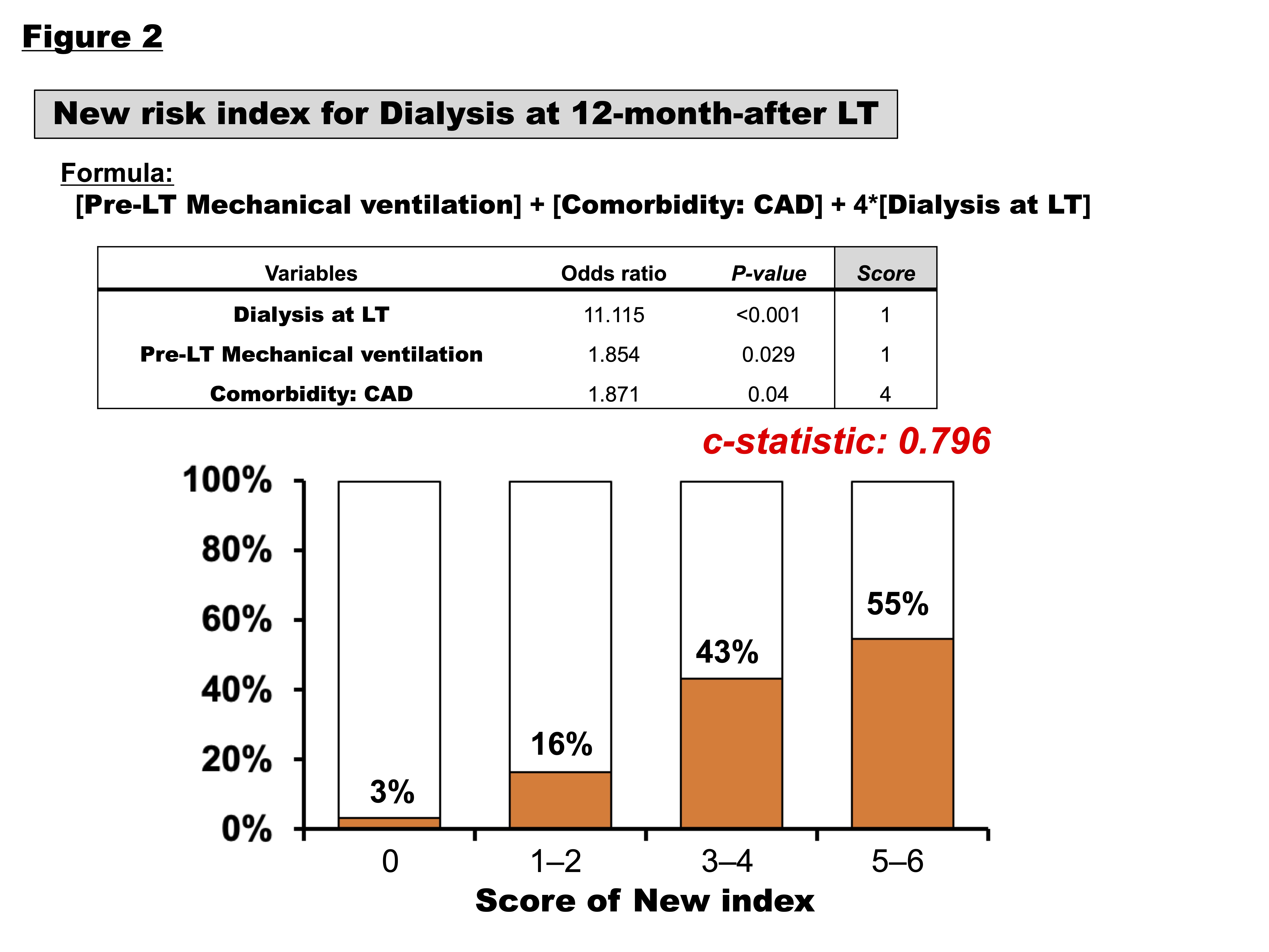
Results: 541 out of 598 patients were included. The physiologic median model for end-stage liver disease (MELD) score was 35. 307 (57%) were on dialysis at time of SLKT or LT. 59 (11%) received SLKT and 31 (6%) eventually received a kidney graft after LT (L-K). Among the SLKT, LTa, and L-K groups, L-K showed a tendency for higher survival rates at 3-year-post-LT (SLKT: 74%, LTa: 83%, L-K: 100%); however, there was no significant difference after 3 years. SLKT and LTa, patients on dialysis at 12M-pLT had significantly lower survival than those not on dialysis (p=0.008 in SLKT, p<0.001 in LTa). Only 32% of LTa patients remaining on dialysis at 12M-pLT ultimately recovered from it (Figure 1A). SLKT had the highest and earliest withdrawal rate from dialysis at 12M-pLT of 96% (LTa: 82%, L-K: 26%, p<0.001). In L-K patients, median wait time for KT was 15 months; ultimately, these patients reached a 100% withdrawal rate post-KT (Figure1B). Multivariate analysis of no SLKT patients identified dialysis at LT (OR 11.115, <0.001), pre-LT mechanical ventilation (OR 1.854, p=0.029), and coronary artery disease (OR 1.871, p=0.04) as independent risk factors for dialysis at 12M-pLT. Based on the OR, we assigned a score for each risk factor and developed a new index (c-statistic 0.796). This index significantly correlated with increased incidence of dialysis 12M-pLT (3% in score 0, 55% in score 5–6, p<0.001).
Conclusion: This analysis examined LT outcomes and dialysis independence with or without KT in the era of the kidney rescue pathway. SLKT had the highest withdrawal rate from dialysis postoperatively. Post-LT dialysis at 12M had lower survival. Independent risk factors for post-LT dialysis at 12M-pLT may serve to guide perioperative management, and kidney graft allocation in high acuity LT recipients.

right-click to download
