Has the risk of liver re-transplantation improved over the two decades? A UNOS data analysis
Michelle H Kim1, Marc L Melcher1, Varvara A Kirchner1, Amy E Gallo1, Clark A Bonham1, Carlos Esquivel1, Kazunari Sasaki1.
1Department of Surgery, Division of Abdominal Transplantation, Stanford University, CA, CA, United States
Introduction: Liver transplantation (LT) is an established treatment option for end-stage liver disease and post-LT outcomes have improved over the two decades. Despite of accumulation of knowledge and improvement of surgical techniques, liver re-transplantation (re-LT) remains a challenging operation, and reported 1-year survival of re-LT is nearly 15% less compared to initial LT in US registry data. Controversy exists regarding indications for re-LT in the context of organ scarcity and the significantly higher chance of organ loss in re-LT. However, re-LT is the only life-saving option for patients with failing liver grafts. The aim of this study was to elucidate whether re-LT outcomes have advanced with experience over the last two decades.
Methods: This study used 134,254 adult patients in the United Network for Organ Sharing (UNOS) database from 2003 to 2020, evaluating the characteristics and outcomes of 6,689 (5.0%) re-LT patients. Re-LT patients were grouped by 3-year intervals to investigate the chronological evolution of re-LT. Postoperative outcomes were evaluated by graft survival (GS) at 30 days, 90 days, and 1-year after transplantation. Cox proportional hazards models were used to assess the hazard ratio (HR) of re-LT. The chronological changes of HRs of re-LT were plotted and compared to donation after cardiac death (DCD) LT.
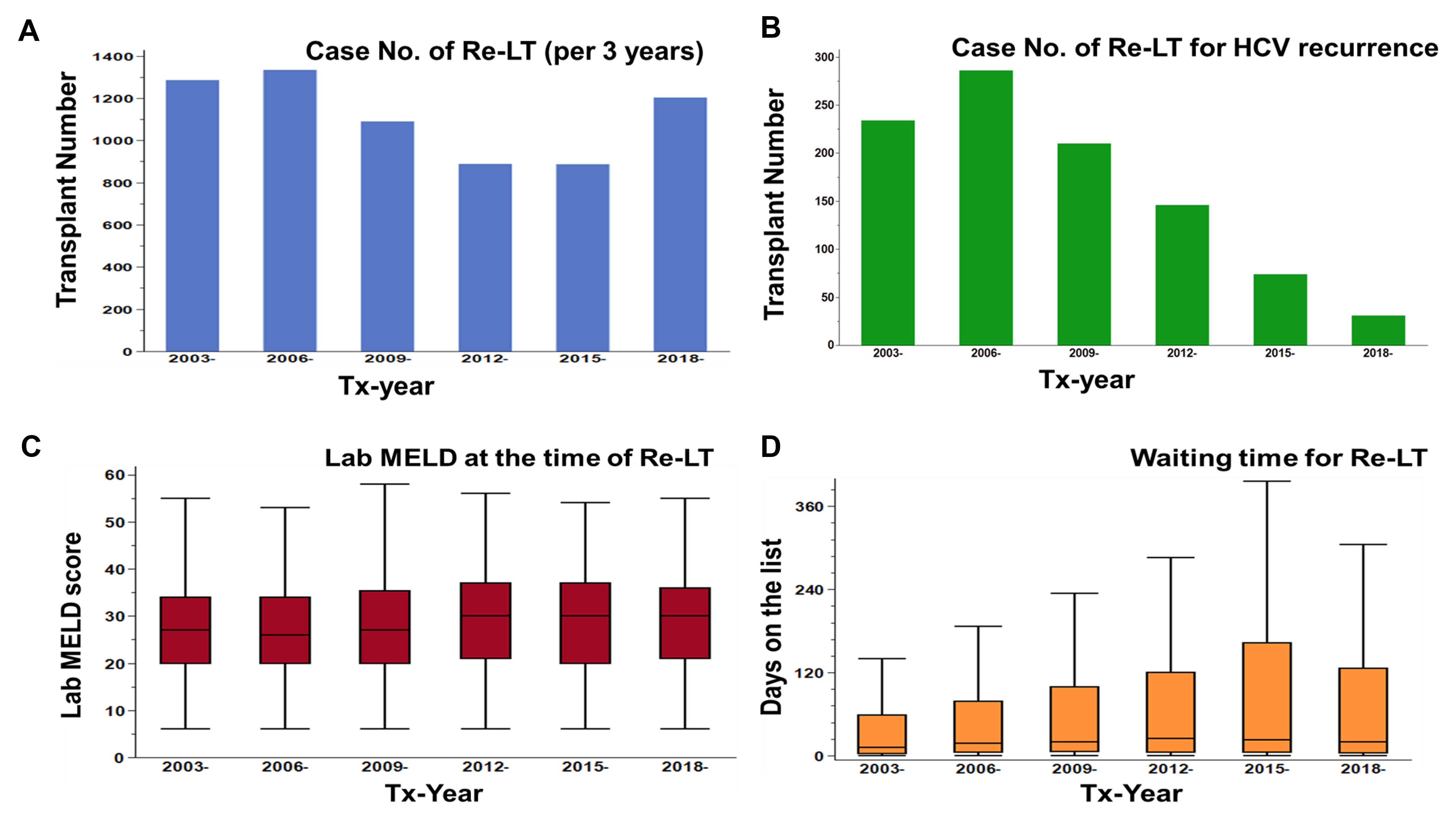
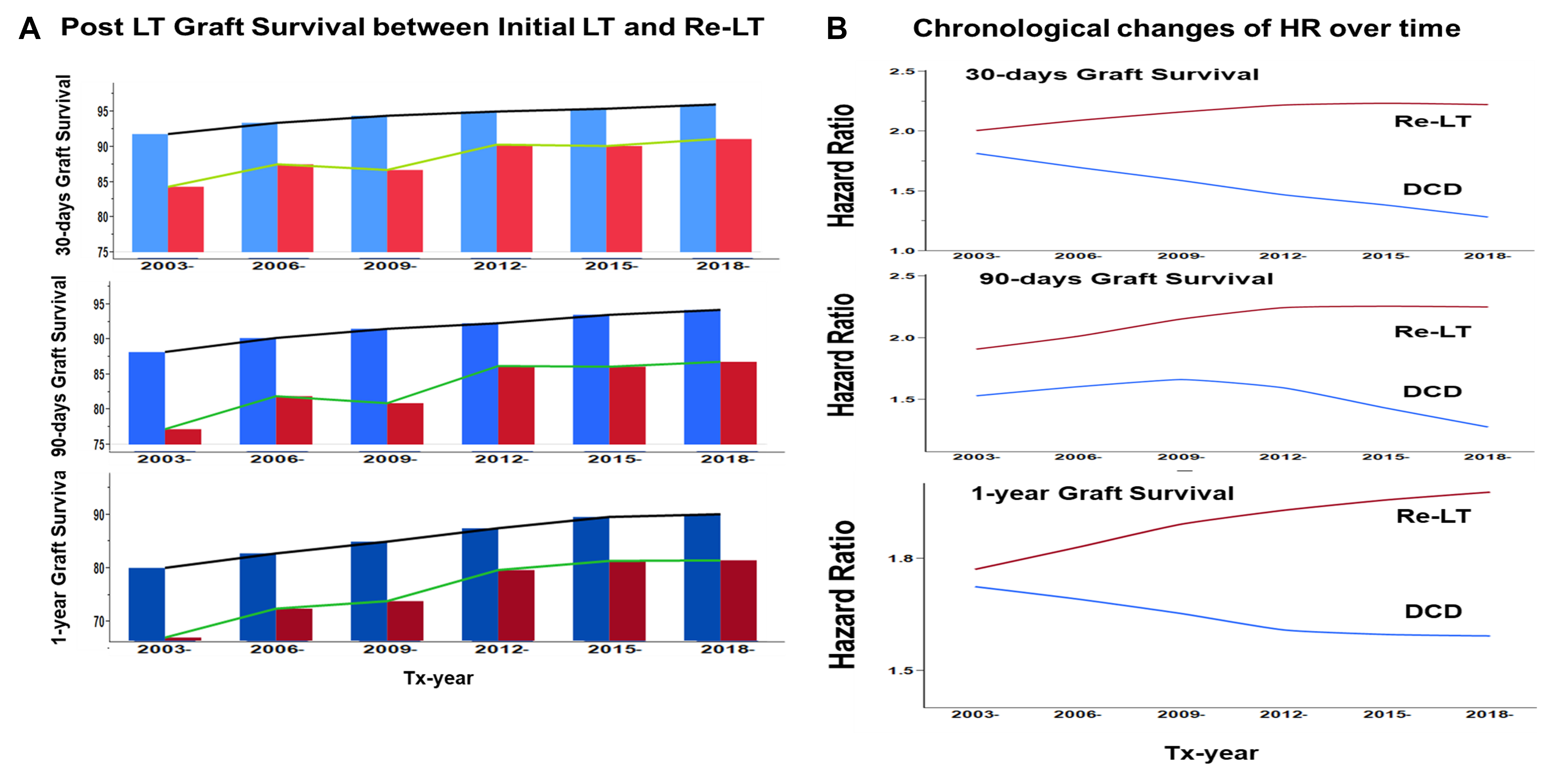
Results: The case numbers of re-LT did not increase over time, despite increases in overall LT volume (Figure 1A). Both waiting time and median MELD at the time of re-LT gradually increased, while the percentage of re-LT for hepatitis C decreased significantly over time (Figure 1B-D). The differences in 30-day, 90-day, and 1-year GS between initial and re-LT decreased over time (2003-2005: 91.7%, 88.1%, and 79.9% vs. 84.2%, 77.1%, and 66.9%, respectively; 2018-2020: 95.9%, 94.1%, and 89.9% vs. 91.0%, 86.7%, and 81.3%, respectively; Figure 2A). The effect of transplant era was examined by comparing HRs between re-LT and DCD LT (Figure 2B). Although graft outcomes of LT using DCD have improved over time, the HR of Re-LT stayed high and did not show clear improvement.
Conclusions: Although GS after re-LT has improved over time, interestingly, the HR of re-LT has not improved with experience. Meanwhile, the HR of using DCD donors in LT has clearly improved over time. These results suggest that the overall re-LT outcomes maybe have improved through strategy optimization in donor-recipient selection, but the adverse prognostic influence of re-LT has not improved despite advancements in LT over the last two decades.

right-click to download
