Inferior long-term outcomes of simultaneous liver-kidney transplantation using donation after cardiac deaths donors in the united network for organ sharing database
Kenji Okumura1, Ryosuke Misawa1, Abhay Dhand1, Sogawa Hiroshi1, Gregory Veillette1, Devon John1, Thomas Diflo1, Seigo Nishida1.
1Surgery, Westchester Medical Center / New York Medical College, Valhalla, NY, United States
Background: Outcomes of simultaneous liver-kidney transplantation (SLKT) in donation after cardiac death (DCD) have improved over the years, but data are limited. Aim of this study was to assess the long-term outcomes of SLKT from DCD organs and then compare them to donation after brain death (DBD) organs.
Methods: We analyzed data from the United Network for Organ Sharing (UNOS) from 2002 to 2021. Adult SLKT were included, other multi-organ and re-transplants were excluded from the analysis. Propensity score matching was performed to assess the outcomes between two groups. P<0.05 was considered as significant.
Results: In the United States, 8733 SLKT were performed during the study period (499 SLKT from DCD and 8234 from DBD). Recipients of DCD organs, when compared to recipients of DBD organs, were older (median age 59 vs 58 years, P=0.005), had lower prevalence of dialysis (62 vs 68%, P=0.003), lower Model for End-Stage Liver Disease (MELD) score (24 vs 29, P<0.001) and longer wait-time (89 vs 68 days, P=0.009). Donors of DCD organs were younger (median age 33 vs 35 years, P<0.001), had shorter cold ischemia time in liver (5.8 vs 6.0 hours, P<0.001) and in kidney (9.5 vs 10.5 hours, P<0.001), and had similar kidney donor profile index (31 vs 30 %, P=0.18) compared to DBD donor. The most common primary diagnosis for both recipient groups was alcohol-related liver disease, while non-alcoholic steatohepatitis was more common in DCD group (28 vs 21%). Long-term outcomes including five-year overall survival and liver graft survivals were inferior in DCD recipients (71.4 vs 74.8%, P=0.11; 74.0 vs 67.1%, P=0.0011). After propensity score matching, five-year overall survival and liver graft survivals were inferior (71.4 vs 76.4%, P=0.031; 67.1 vs 76.0%, P<0.001). Multivariable cox-regression analysis in the matched-cohort showed that DCD was an independent risk factor of mortality (hazard ratio {HR}- 1.33; 95% Confidence interval{CI}, 1.04-1.68; P=0.021) and liver graft failure (HR- 1.54; 95% CI, 1.24-1.92; P<0.001). For kidney allograft outcomes in matched-cohort, delayed graft function was higher in DCD (36 vs 20%, P<0.001) and five-year kidney graft outcome was inferior in DCD (67.3 vs 74.7%, P=0.0034). The most common listed causes of five-year mortality were infection (21.4%) and multi-organ failure (20.8%) and there were no differences between two groups. Other factors associated with mortality were recipient older age (HR 1.03; 95%CI 1.02-1.04, P<0.001), male recipient (HR 1.32; 95%CI 1.06-1.64, P=0.014), and donor older age (HR 1.01; 95%CI 1.00-1.02, P=0.024).
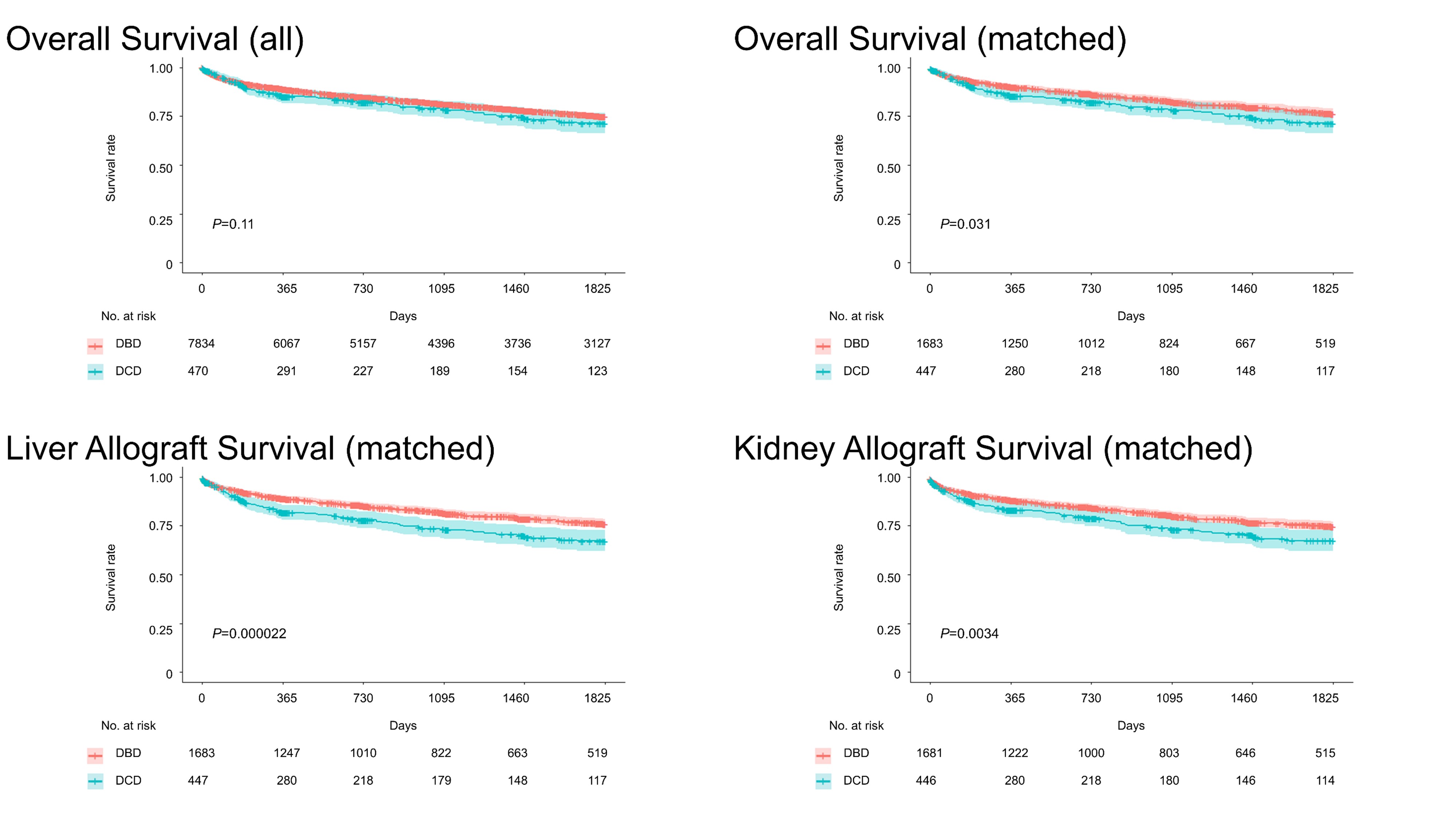
Conclusion: Recipients of SLKT from DCD donors had inferior long-term post-transplant outcomes with decrease in overall survival and allograft survival. Careful identification of risk factors associated with worse outcomes is required to improve utilization of DCD donors for SLKT.

right-click to download
