What is the risk factor of graft mortality in patients who underwent simultaneous splenectomy during living donor liver transplantation?
Tomoharu Yoshizumi1, Noboru Harada1, Takeo Toshima1, Kazuki Takeishi1, Kazutoyo Morita1, Yoshihiro Nagao1, Shohei Yoshiya1, Shinji Itoh1.
1Department of Surgery and Science, Kyushu University, Fukuoka, Japan
Introduction: Splenectomy is performed in living donor liver transplantation (LDLT) for portal flow modulation. The aim of this study was to identify the risk factor of 6-month graft mortality in patients who underwent splenectomy in LDLT.
Methods: Data from 441 adult patients who underwent simultaneous splenectomy during primary LDLT were collected retrospectively. Risk factors of 6-month graft mortality were investigated.
Results: Mean recipient age was 55 years. Mean donor age was 38.7 years. Two hundred and five patients (46.5%) received left lobe graft. Mean graft weight (GW)-standard liver weight ratio was 41.5% and GW-recipient weight ratio was 0.79%. Six-month graft survival rate after LDLT in 441 patients was 93.8%, which was significantly better compared to patients without simultaneous splenectomy or splenic artery ligation (83.9%, p<0.0001). Univariate analysis revealed the following risk factors for 6-month graft mortality in patients with splenectomy: neutrophil-lymphocyte ratio > 4, acute liver failure, hospitalized before LDLT, donor > 60 years of age, MELD score > 22, pre-LDLT platelet < 40, 000/mm3, portal vein pressure when LDLT finished (PVP) > 20 mmHg. Multivariate analysis identified that donor > 60 years of age (Hazard ratio=4.50, p=0.049), pre-LDLT platelet < 40, 000/mm3 (Hazard ratio=2.58, p=0.03), and PVP > 20 mmHg (Hazard ratio=7.46, p<0.001) were the independent risk factors of 6-month graft mortality after LDLT.
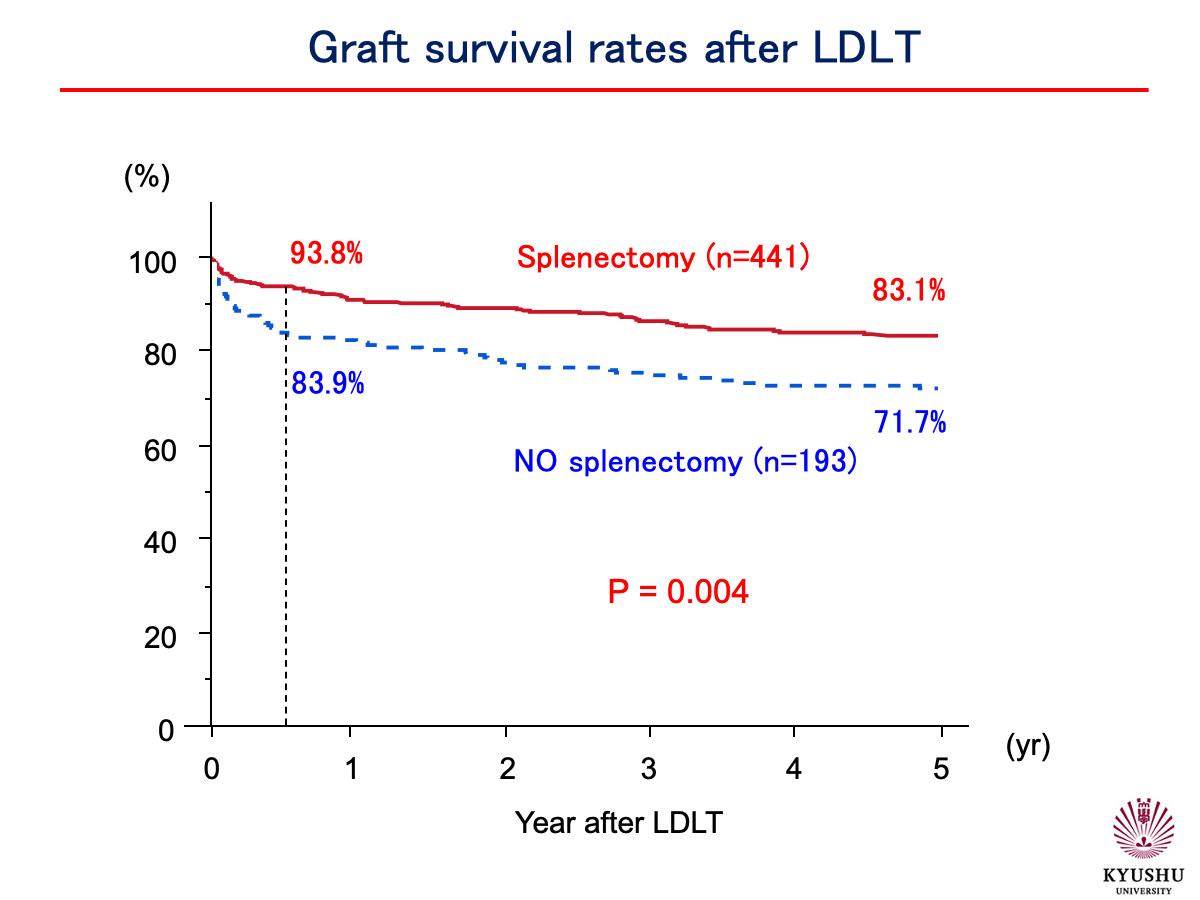
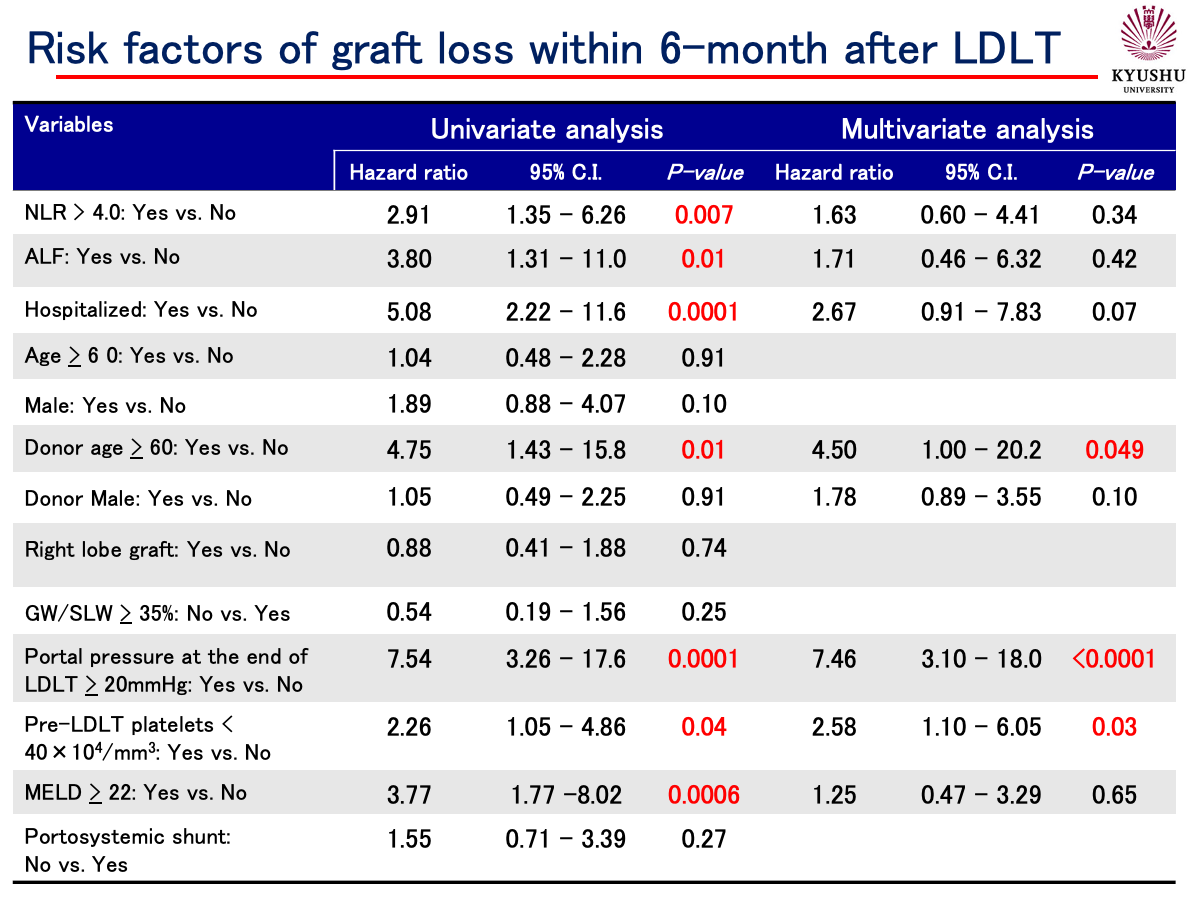
Conclusion: Splenectomy in LDLT improves survival rate after LDLT. Careful attention is needed for patients with platelet < 40, 000/mm3, PVP > 20 mmHg, and received graft from donor > 60 years of age.

right-click to download
