Inadequate iodine intake and long-term outcomes after kidney transplantation
Yvonne van der Veen 1, Daan Kremer1, Adrian Post1, Daan J. Touw2, C. Annema3, Casper F.M. Franssen1, Stephan J.L. Bakker1.
1Internal Medicine, section of Nephrology, University Medical Center Groningen, Groningen, Netherlands; 2Clinical Pharmacy and Pharmacology, University Medical Center Groningen, Groningen, Netherlands; 3Health Sciences, section of Nursing Sciency, University Medical Center Groningen, Groningen, Netherlands
Objective: There is a great need for identification of novel modifiable factors to decrease the risk of graft failure and premature mortality in kidney transplant recipients (KTR). We hypothesized that inadequate iodine intake may be one of these modifiable factors. Severe iodine deficiency as a public health problem is now largely under control worldwide, thanks to the introduction of iodized salt in the 1920s. However, for KTR, salt intake may be significantly reduced due to a salt-restricted diet both before and after transplantation, potentially also resulting in inadequate intake of iodine. We aimed to investigate the prevalence and potential determinants of inadequate iodine intake among KTR. In addition, we assessed potential repercussions of inadequate iodine intake, by assessing its associations with graft failure and mortality.
Methods: We determined 24h urinary iodine excretion by means of inductively-coupled plasma mass spectrometry in stable outpatient KTR, enrolled in the TransplantLines Food and Nutrition Biobank and Cohort Study. Inadequate iodine intake was defined as a 24-h urinary iodine excretion <150 µg. Dietary intake was assessed using validated 177-item food-frequency questionnaires. We aimed to identify potential determinants of inadequate iodine intake using logistic regression. In addition, we assessed the prospective association of inadequate iodine intake with graft failure and all-cause mortality using uni- and multivariable Cox regression analysis.
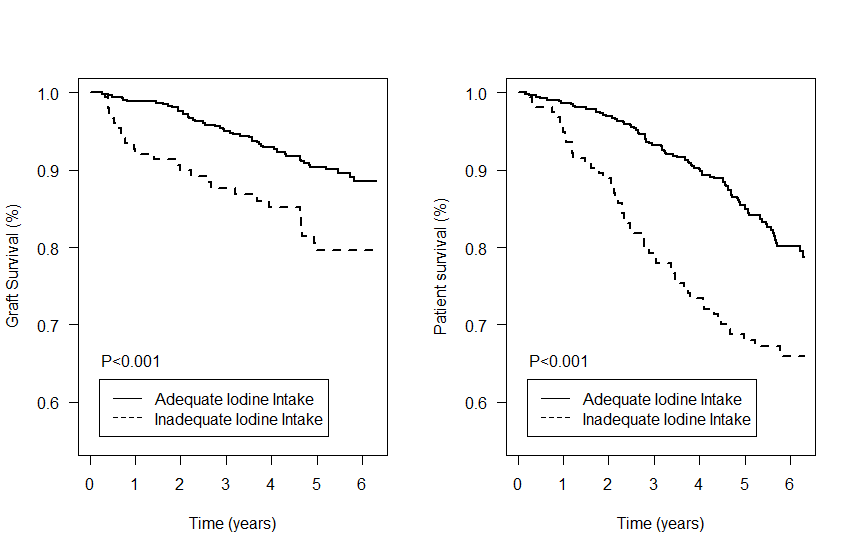
Results: In total, we included 668 KTR (43.4% female, age 53 ± 13 years), at 5.7 [IQR: 2.2 to 12.2] years after transplantation. Median 24h urinary iodine excretion was 201 [IQR: 153 to 266] µg, and 154 (23%) KTR had inadequate iodine intake. Low body height, low urinary sodium excretion, and low intake of bread, eggs, and animal protein were identified as key determinants of inadequate iodine intake. Univariable Cox regression analyses showed that inadequate iodine intake was strongly associated with higher risk of graft failure (HR per doubling: 2.16, 95%CI: 1.36 to 3.43, P=0.001) and mortality (HR per doubling: 2.05, 95%CI: 1.46 to 2.89, P=<0.001).These associations remained materially unchanged after adjustment for age, sex, height, weight, eGFR, 24h urinary protein excretion, HLA class II antibodies, energy intake, urinary sodium excretion, and free T3.
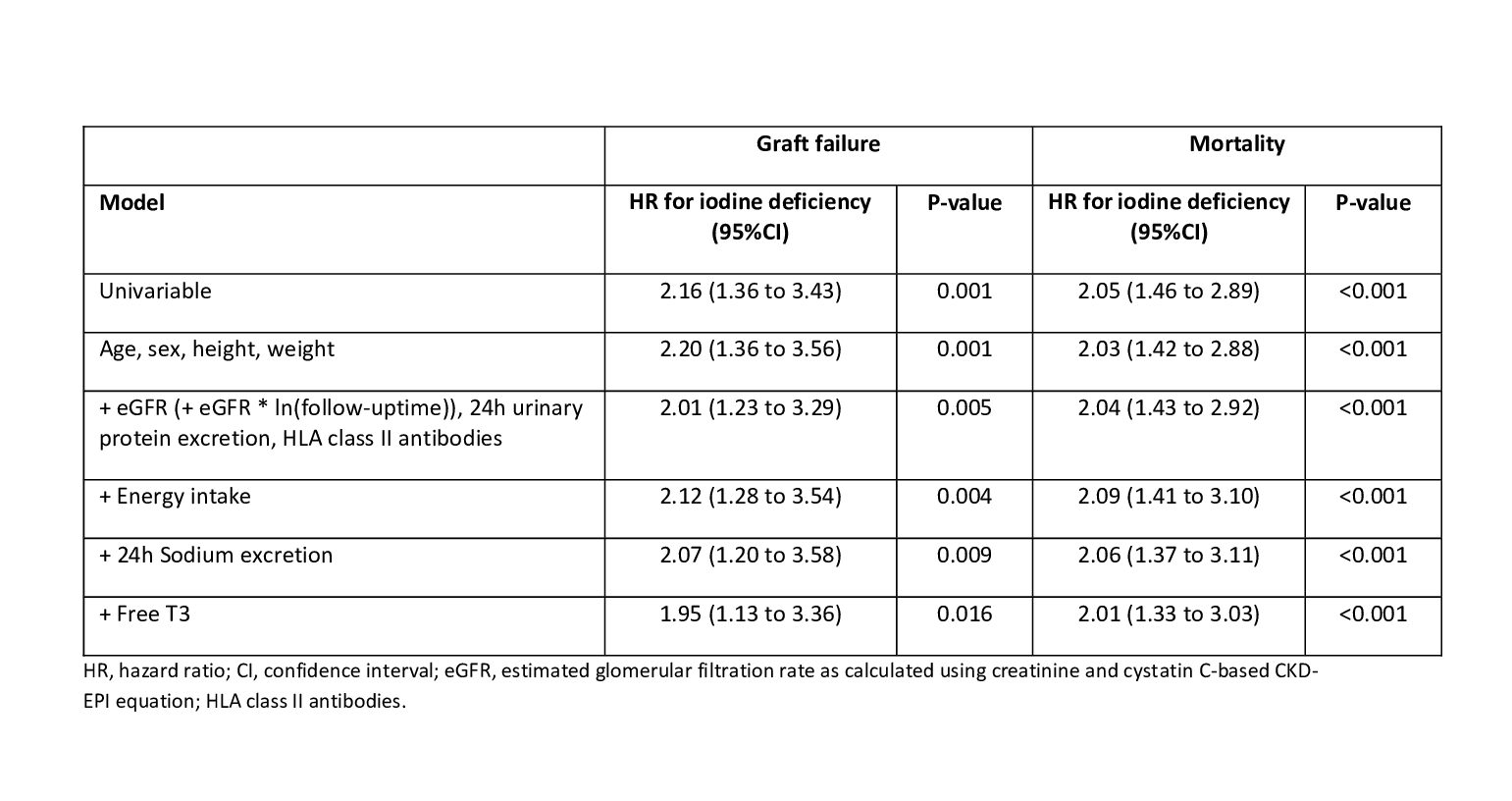
Conclusion: Inadequate iodine intake is prevalent among KTR, and its occurrence appears to be strongly related to dietary factors, including salt intake. Inadequate iodine intake was strongly and independently associated with an increased risk for graft failure and all-cause mortality. These results suggest that supplementation of iodine may reduce risks of graft failure and premature mortality among KTR. Interventional trials are necessary to confirm the potential of stimulating dietary iodine intake or iodine supplementation in KTR.

right-click to download
