Clinical outcomes among patients with Autosomal Dominant Polycystic Kidney Disease (ADPKD) submitted to kidney transplant compared with a non-ADPKD paired group: a propensity score matched cohort study
Letícia Y Okabe1, Renato D Foresto1,2, Lúcio Requião-Moura1,2, José Medina-Pestana1,2.
1Nephrology Division, Universidade Federal de São Paulo, São Paulo, Brazil; 2Hospital do Rim, Fundação Oswaldo Ramos, São Paulo, Brazil
Background: Beyond the kidney function impairment, the autosomal dominant polycystic kidney disease (ADPKD) patients present abnormal kidney volume, impacting the abdominal venous capacity and the sympathetic/parasympathetic control, which would hypothetically affect early outcomes after kidney transplant (KT). Thus, this study aimed to evaluate whether ADPKD is associated with early outcomes after KT, focused on delayed graft function (DGF).
Methods: This single-center cohort study enrolled 245 patients with ADPKD transplanted from a deceased donor between 2013-17. The control group comprised non-diabetic patients transplanted in the same period (n= 2,596). The analyses were provided before and after a 1:2 propensity score matching. The primary outcome was DGF. Logistic regression was performed to evaluate the variables associated with DGF.
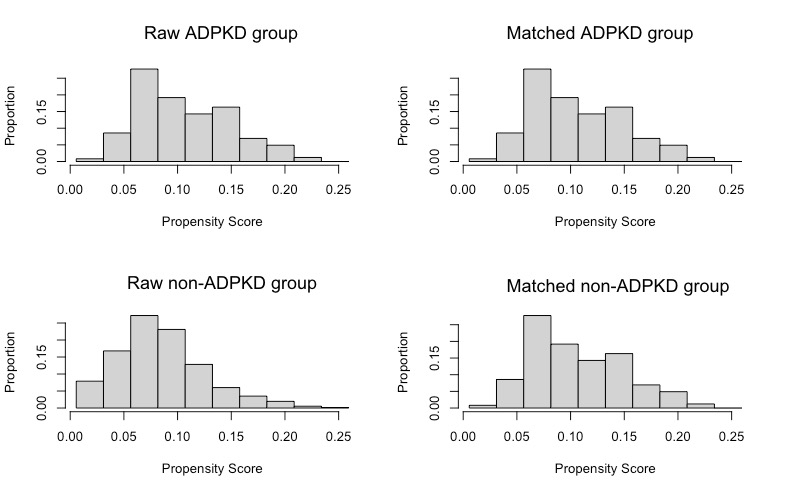
Results: In the ADPKD-group, recipients were older (57 vs. 49 years, p<0.001), more frequently female (51% vs. 37%, p<0.001), and candidate for a first KT (98.4% vs. 92.1%, p<0.001). Before matching, the frequency of DGF was significantly lower among ADPKD-group, 52.2% vs. 60.5% (p=0.012), for whom the time in DGF tended to be shorter (2 vs. 6.5 days, p=0.41). In the multivariable model, the variables associated with the probability of DGF were: male recipients (OR=1.25; p=0.01) and male donors (OR=1.39; p<0.001); hemodialysis as RRT previous to the KT (OR= 1.58; p<0.001) and time waiting for the KT (OR=1.06; p<0.001); KDPI (reference[1-35%], OR[35-51%]=1.47, P=0.01; OR[51-80%]=1.82, P<0.001; and OR[>85%]=1.83, p<0.001); and cold ischemia time (OR=1.02; p<0.001). The ADPKD tended to reduce the probability of DGF: OR=0.76, P=0.05. There were no differences in the 1-yr rate of death, 2.9% vs. 3.3% (p=0.71), and graft loss, 4.1% vs. 4.8% (p=0.62) for ADPKD and control groups, respectively. However, the graft loss due to thrombosis was more frequent in the ADPKD-group: 50% vs. 33%, p=0.02. After the propensity score matching, the frequency of DGF was 52.2% in ADPKD-group vs. 56.5% in the control group (OR= 0.84, p=0.27), with no difference in time in DGF. There were also no differences in the 1-yr rate of death, 2.9% vs. 2.7% (P=0.87), and graft loss, 4.1% vs. 5.3% (P=0.47); however, the graft loss due to thrombosis remained more frequent in the ADPKD-group: 50% vs. 34.6%.
Conclusions: There was no association between ADPKD and; however, as before, as well as after matching, ADPKD recipients presented a significantly higher frequency of graft loss due to vascular thrombosis, despite a low frequency of events.

right-click to download
