Which patients over 60 years old are candidates for a kidney transplant? Usefulness of a mortality predictive score
Pehuén Fernández1,2,3, Facundo Schwarz1,3, Juan Pablo Maldonado1,3, Martín Cheballier1,3, Esteban Metrebian1, Andrés Parisi1, Walter Douthat1,2,3, Javier De Artega1,2,3, Carlos Chiurchiu1,2,3, Jorge De La Fuente1,2,3.
1Renal Transplant Program, Hospital Privado Universitario de Córdoba, Córdoba, Argentina; 2Instituto Universitario de Ciencias Biomédicas de Córdoba (IUCBC), Córdoba, Argentina; 3Postgraduate School in Nephrology, Universidad Católica de Córdoba (UCC), Córdoba, Argentina
Introduction: The decision to indicate a kidney transplant (KT) to an elderly patient with end-stage chronic kidney disease is not simple due to the high morbidity and mortality associated. The Dusseux et al. score was originally developed in France to predict 3-year post kidney transplant mortality in subjects older than 70 years. The objective of this study was to evaluate the usefulness of this score to predict 1-year post KT mortality in patients older than 60 years and to identify the best cut-off point.
Methods: A retrospective cohort study was performed. All patients over 60 years old who received a KT at Hospital Privado Universitario de Córdoba between January 2009 and December 2015 were consecutively included. A one-year post-KT follow-up was carried out and variables associated with mortality were analyzed. The Dusseux et al. score considers as predictive variables: sex, age, etiology of chronic kidney disease, comorbidities, mobility status, body mass index and the presence of a temporary catheter at the time of dialysis initiation. The t test or Mann-Whitney test were used to evaluate differences between continuous variables t, and chi2 or Fisher's test for categorical variables, as appropriate. To evaluate the predictive capacity, the area under the curve (AUC) was used and the Youdex Index J was applied to identify the best cut-off point, with its sensitivity and specificity. Kaplan Meier survival curves were made and then compared with the logRank test. A value of p<0.05 was considered statistically significant.
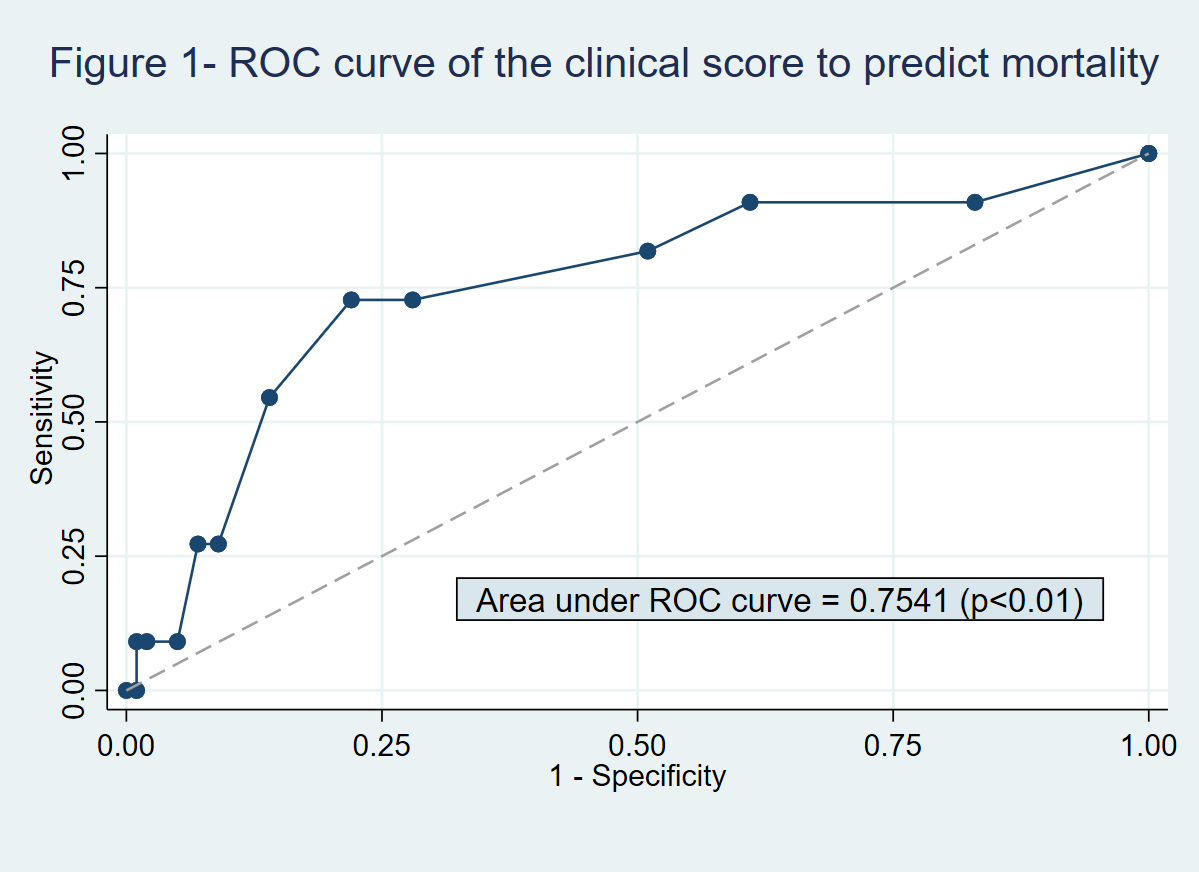
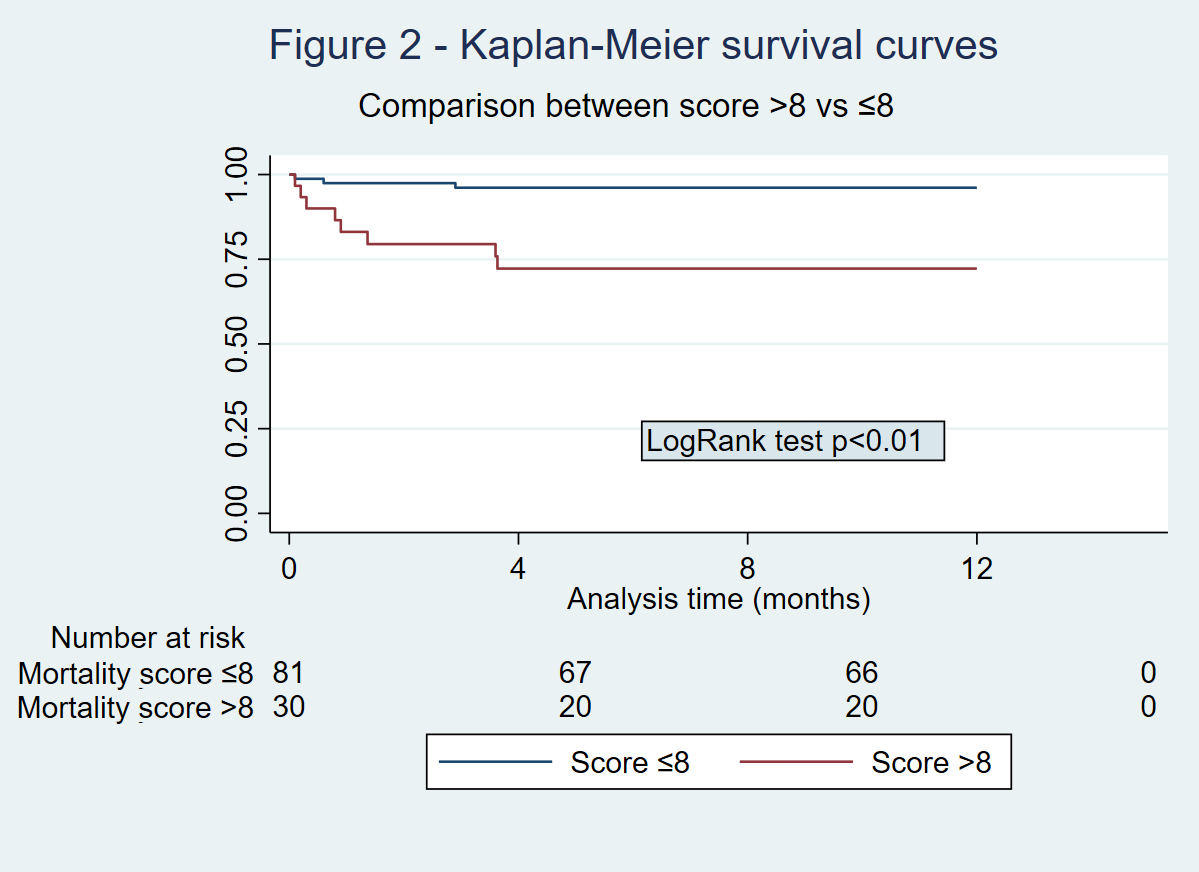
Results: We included 111 patients aged 66.2 ± 5.2 years, 54.9% were men. As relevant comorbidities, 30.7% were diabetic and 13.5% had ischemic heart disease. 82% received a cadaveric KT. As induction, 100% were given steroids, 60.3% basiliximab, 22.5% thymoglobulin and 9.9% gamma globulin. As maintenance, 93.7% were treated with steroids, tacrolimus and mycophenolate. Mortality during follow-up was 9.9% (n:11; 8 due to infectious etiology and 3 from cardiovascular disease). The patients who died were older (70.3 ± 6.6 vs 65.8 ± 4.9; p=0.05), had a greater history of ischemic heart disease (36.7% vs 11%; p=0.04), and had a higher mortality predictive score (9.4 ± 3 vs 6.8 ± 2.5, p=0.02). There were no differences in the rest of the variables. This score obtained a high AUC to predict mortality (AUC=0.75; p<0.01; figure 1) and the best cut-off point was 8, with a sensitivity of 72.7% and a specificity of 78%. Subjects with a score >8 had higher mortality than those with a score ≤8 (26.7% vs 3.7% respectively; p<0.01). There were significant differences between the survival curves of these groups (p<0.01; figure 2).
Conclusion: This clinical score is a good predictor of mortality 1-year after KT in patients over 60 years old. The best cut-off point of the score was 8 points. This could be a useful and simple tool to help in the decision to indicate a KT in this type of patients.
Fundación Nefrológica de Córdoba.

right-click to download
