
Selective ureteric stenting is non-inferior to routine stenting for major urological complications following renal transplant in low-risk patients
Dylan Barnett1,2, Zihong Kuah1, Vidyasagar Kallepalli1, Santosh Olakkengil1, Shantanu Bhattacharjya1,2.
1Central and Northern Renal and Transplantation Service (CNARTS), Royal Adelaide Hospital, Adelaide, Australia; 2Department of Surgery, University of Adelaide, Adelaide, Australia
Introduction: Major urological complications (MUC) are a significant source of morbidity following a renal transplant occurring in up to 4% of cases. At our institution it has been standard practice to routinely place a J-J ureteric stent across the ureteroneocystostomy at the time of transplant. Meta-analysis has shown reduced incidence of MUC in randomised-controlled trials of stenting with a number needed to treat of 14 to prevent 1 MUC. Despite the potential benefits of routine stenting, evidence suggests there may be no statistical difference between routine vs. selective stenting for low-risk patients in terms of complications such as urinary leak and ureteric obstruction suggesting equipoise for this sub-group. Also, stenting itself is associated with several complications and increased costs such as urinary tract infection (UTI), BK virus and the need to retrieve the stent through flexible cystoscopy. We hypothesised that in select low-risk patients not stenting would be non-inferior to routine stenting in the remainder of our patients.
Study design: After local ethics approval, our prospective observational cohort study was run between June 2017 and June 2021. In this period 380 consecutive renal transplants were performed at our centre. 30 patients were excluded who had dual kidney (including paediatric en bloc) transplant, early graft loss not related to a MUC, duplex ureter in the donor or an intra-peritoneal implantation. Following this, 350 transplants were included for analysis, 240 were stented and 110 were not. Primary outcomes were MUC and UTI and secondary outcome was the incidence of BK viraemia.
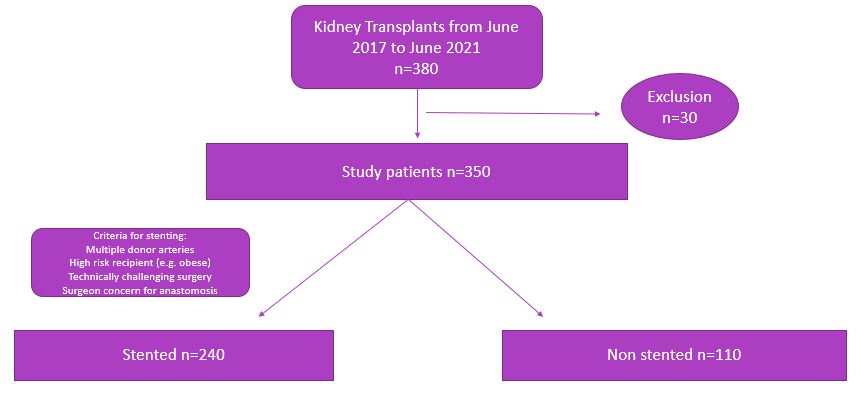
All transplants used the same technique for ureteroneocystostomy, the Lich-Gregoir anti-refluxing anastomosis. The same 3 surgeons performed or directly supervised each transplant. The decision of whether to stent was at the discretion of each surgeon based on suggested criteria. Stenting was suggested for multiple donor renal arteries, technically difficult surgery, high risk (e.g. obese) patients or surgeon concerns regarding the ureteric anastomosis. A 5Fr Cook UniversaTM ureteric stent was used when stenting was performed. Patients were followed from transplant for a minimum of 6-months.
Results: MUC occurred in 6.25% of stented vs. 7.2% of the not stented groups. These included early (<10 days) and late urinary leak, haematuria requiring washout, hydronephrosis requiring nephrostomy and stent encrustation. Observed rates of urinary tract infection (28.7% vs. 26.3%) and BK viraemia (8.7% vs. 8.1%) were similar between groups.
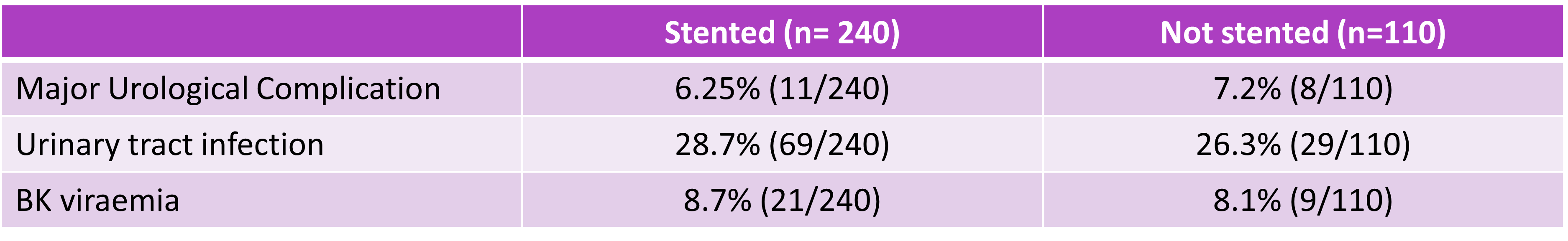
Conclusions: In our cohort of 350 renal transplants, selectively stenting low-risk patients did not result in a higher rate of MUC. Rates of UTI or BK viraemia were not significantly different. Finally, not needing to remove a stent in our selective group was associated with savings of an estimated $165,000 AUD over 3 years with no statistically significant difference in complications.

right-click to download
