Post-transplant lymphoproliferative disorders after solid organ and hematopoietic stem cell transplantation: a nationwide cohort study in Korea
Kyong Ihn1,2,3, Seung Min Hahn4, Myeongjee Lee5, Eun Hwa Kim5, Ji-Man Kang6, Sung Min Lim6, Dong Jin Joo1,2, Inkyung Jung7.
1Division of Transplantation Surgery, Severance Hospital, Yonsei University Health System, Seoul, Korea; 2Department of Surgery, Yonsei University College of Medicine, Seoul, Korea; 3Division of Pediatric Surgery, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Korea; 4Division of Pediatric Hematology & Oncology, Department of Pediatrics, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea; 5Biostatistics Collaboration Unit, Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea; 6Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea; 7Division of Biostatistics, Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea
Introduction: Post-transplant lymphoproliferative disorders (PTLD) are the majority of cancer diagnoses after solid organ transplantation (SOT) and allogeneic hematopoietic stem cell transplantation (HSCT) with a high incidence of PTLD developed in the first post-transplant year. However, there is minimal nationwide literature examining the incidence and risk analysis of PTLD. We investigated the incidence and risk determinants of PTLD in Korean SOT and HSCT recipients using a large national database.
Method: This study recruited 47,708 patients (SOT: 37,023; HSCT: 10,685) from the Korean National Health Insurance Service database between 1 January 2009 and 31 December 2020. Patients previously diagnosed with hematologic or lymphoproliferative malignancies or multi-organ transplant recipients were excluded.
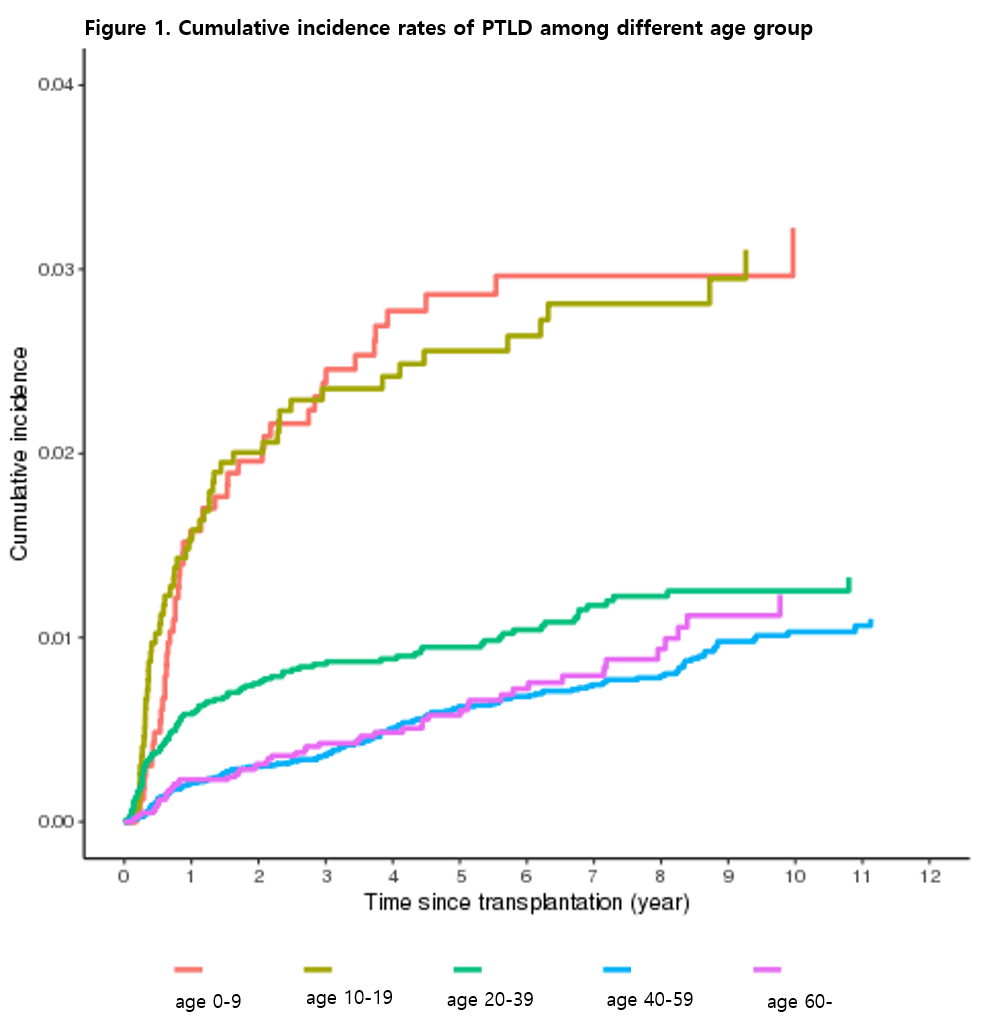
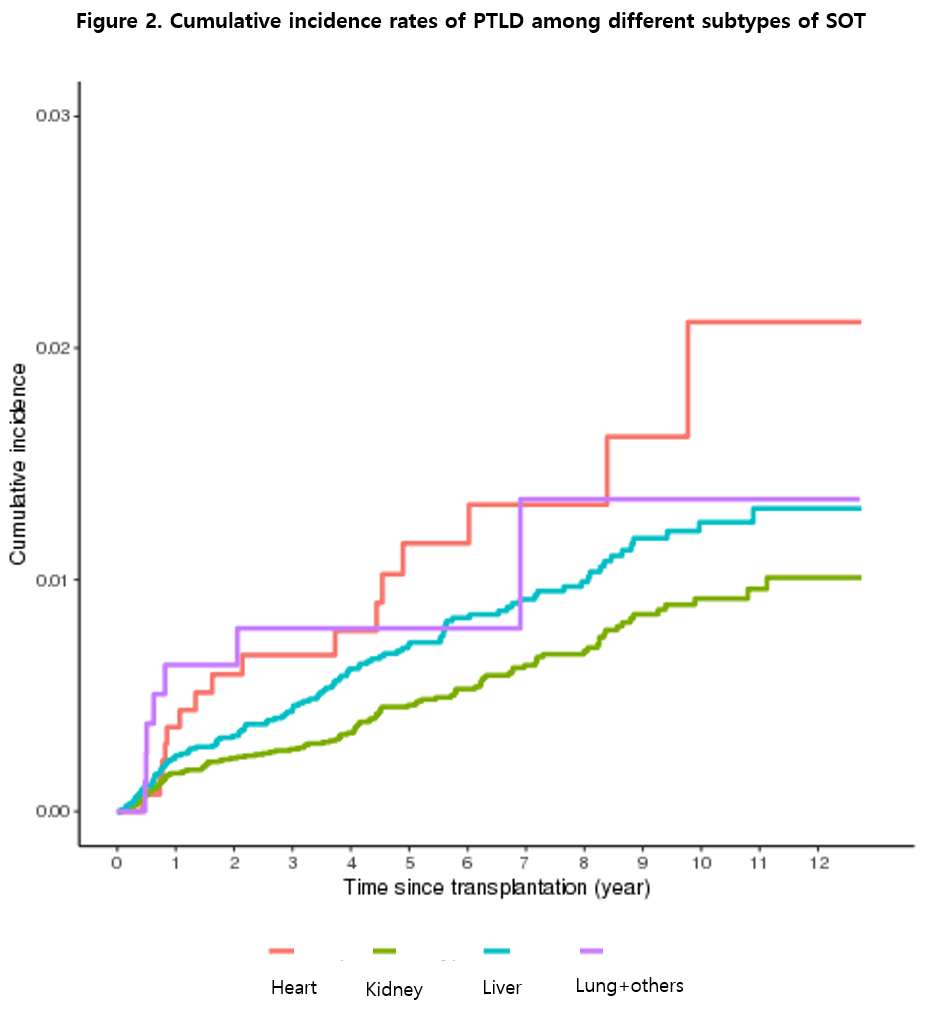
Results: PTLD developed in 432 patients (SOT: 257; HSCT: 175). According to the type of transplant, PTLD after HSCT was the most common (1.64%), followed by heart (1.16%), lung (0.98%), liver (0.83%), kidney (0.57%). The subdistributional hazard ratio (SHR) of PTLD in pediatric patients younger than 9 years of age was higher than that in those aged 20 to 39 years (SHR: 2.184, p < 0.001, 95% confidence interval [CI]: 1.490-3.201). When compared with SOT, HSCT was associated with a greater risk of PTLD (SHR: 1.833, p < 0.001, 95% CI: 1.461-2.299). The hazard ratio (HR) of death after diagnosing PTLD in patients aged over 60 years was higher than that in those aged 20 to 39 years (HR: 2.612, p < 0.001, 95% CI: 2.411-2.830). When compared with SOT. HSCT was associated with a greater risk of death after PTLD (HR 5.075, p < 0.001, 95% CI: 4.829-5.332).
Conclusion: This nationwide population-based cohort study revealed that PTLD was associated with a higher risk of pediatric age, especially in the 0-9 years age group. According to the type of transplantation, HSCT was at greater risk of developing PTLD and death after the diagnosis of PTLD than SOT.

right-click to download
