Dietary protein intake and blood pressure after living kidney donation
Ekamol Tantisattamo1, Natchaya Polpichai2, Watsachon Pangkanon3, Phuuwadith Wattanachayakul4, Chawin Lopimpisuth5, Pakin Lalitnithi5, Pornthira Mutirangura6, Manasawee Tanariyakul5.
1Division of Nephrology, Hypertension and Kidney Transplantation, Department of Medicine, University of California Irvine School of Medicine, Orange, CA, United States; 2Faculty of Medicine Songklanagarin Hospital, Prince of Songkla University, Songkhla, Thailand; 3Faculty of Medicine, Srinakharinwirot University, Bangkok, Thailand; 4Department of Microbiology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand; 5Faculty of Medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand; 6Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Background: High dietary protein intake is associated with worsening kidney function especially in at-risk patients such as living kidney donors; high blood pressure is a known risk factor for kidney disease. Whether pre-donation protein intake contributes to post-donation blood pressure is unknown.
Methods: A single-center cohort study included living kidney donors undergoing living kidney donation in 2021 and divided the patients into 2 groups: low and high pre-donation protein intake defined by dietary protein intake estimated from 24-hour urine collection <1 (LPI) and ≥1 (HPI) g/kg/day, respectively. Association between dietary protein intake and systolic blood pressure during the first two weeks post-donation was evaluated by multiple linear regression.
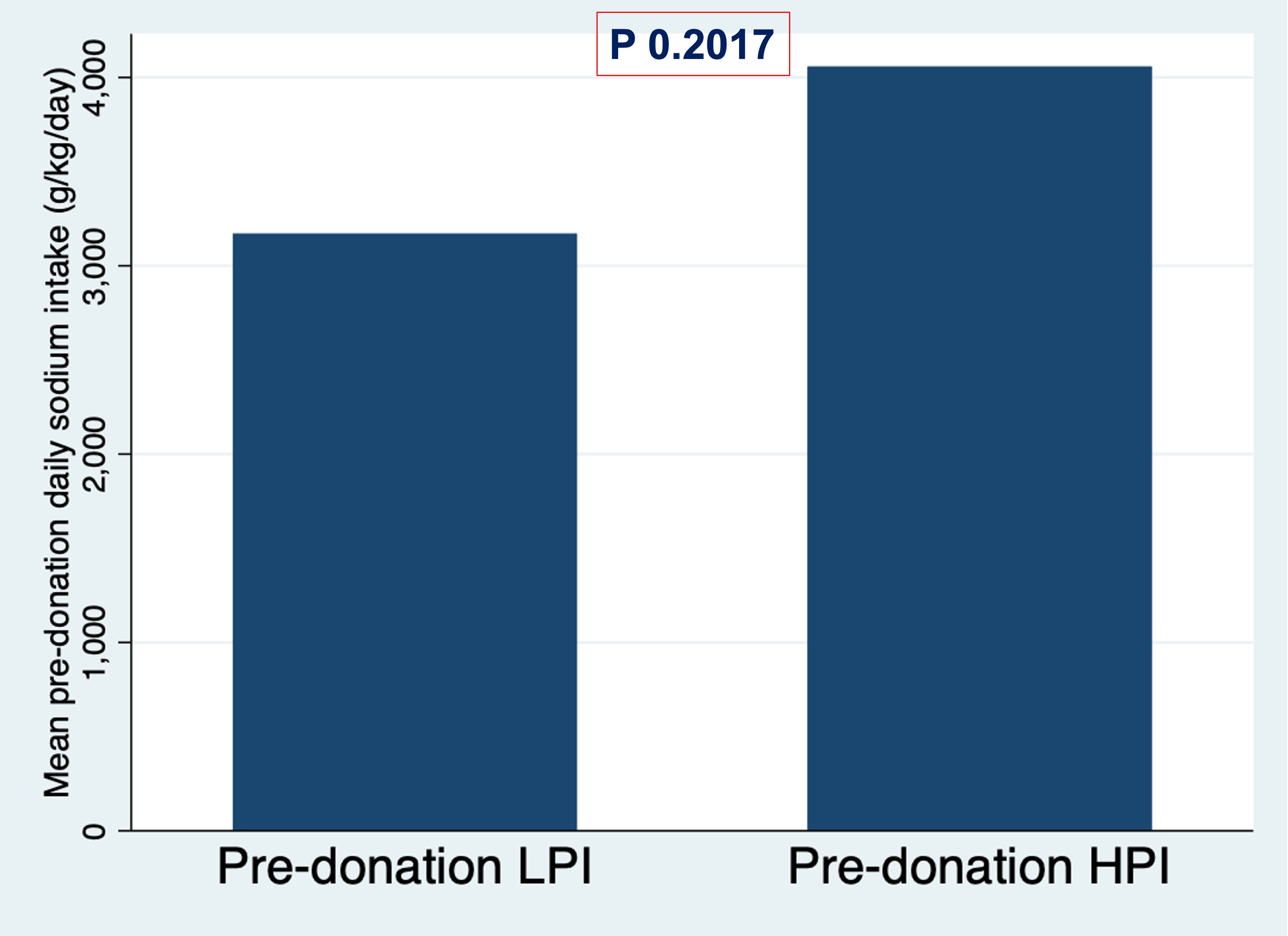
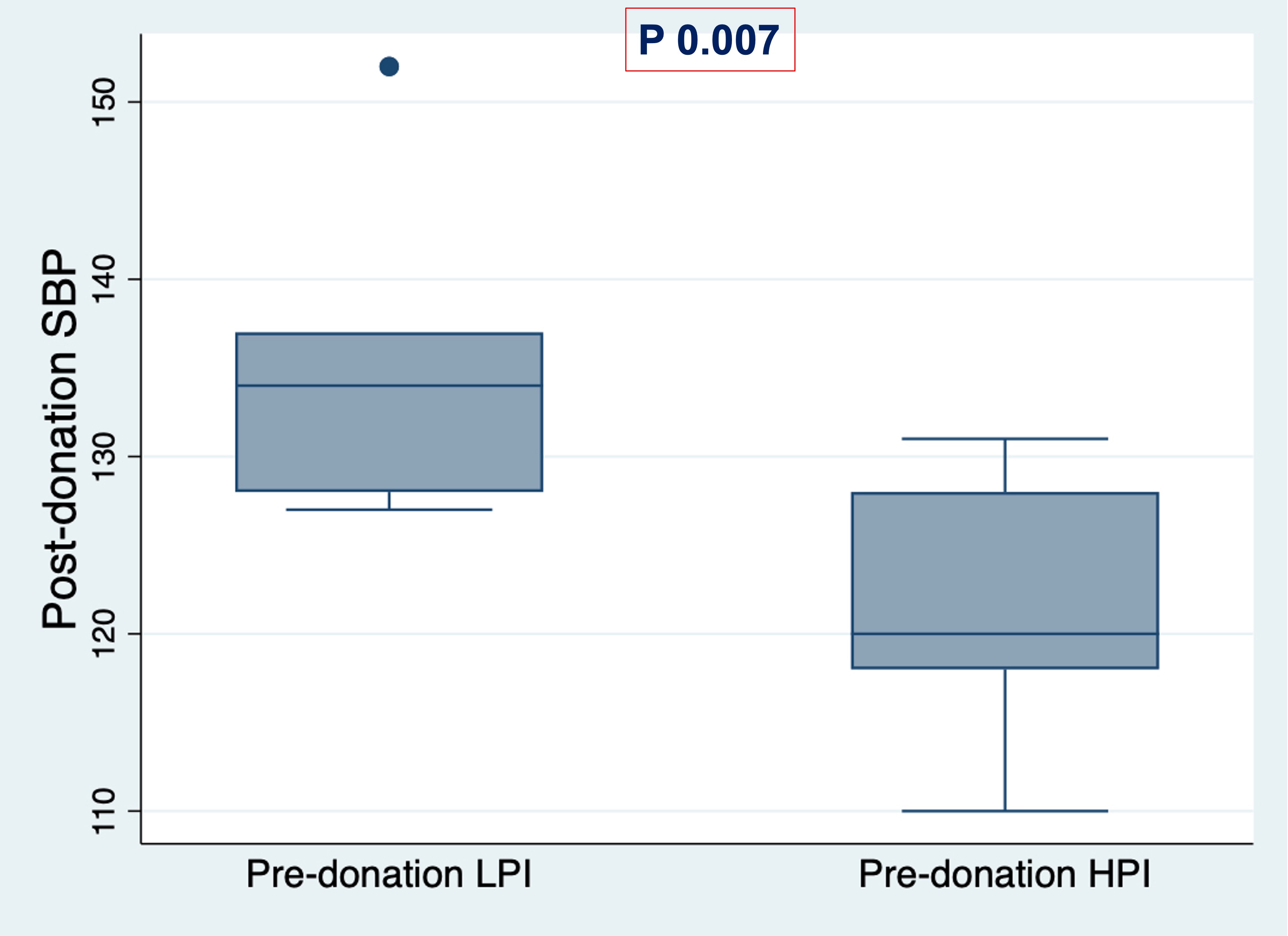
Results: Of 14 living kidney donors, mean±SD was 44±12 and 50% were female. Half of the study population were in the LPI group with a mean dietary protein intake of 0.8±0.1 g/kg/day and the remaining seven patients in the HPI group had a dietary protein intake of 2.2±2.5 g/kg/day (meandifference HPI vs LPI 1.4; p 0.172; 95%CI -0.7, 3.5). Dietary sodium intake was not different between the two groups (mean sodium intake of LPI 3,171±1,315 and of HPI 4,058±1,135 g/day, meandifferenc HPI vs LPI 887; p 0.202; 95%CI -544, 2,318; Figure 1). Mean systolic blood pressure of LPI and HPI groups were 135±8 and 121±7 mmHg, respectively (meandifference LPI vs HPI 14; p 0.007; 95%CI 5, 23). Compared to the LPI group, the HPI group had 14 mmHg lower systolic blood pressure (β -14; p 0.007; 95%CI -23, -5; Figure 2). After adjusted by age, gender, ethnicity, pre-donation body mass index, dietary sodium intake (<4 vs ≥4 g/day), and the interaction term between dietary protein intake and dietary sodium intake, the magnitude and direction of the association between dietary protein intake and systolic blood pressure remain the same (β -13, p 0.043, 95%CI -26, -0.6) and dietary sodium intake did not modify the association (Pinteraction 0.498).
Conclusions: Higher dietary protein intake during pre-donation is inversely associated with SBP level without the effect of dietary sodium intake. Although HPI is associated with adverse kidney outcomes, the protective association between HPI and high blood pressure may involve physiological change after donor nephrectomy and further studies with long-term follow-up are required.

right-click to download
