Salt sensitivity in living kidney donors: a new cardiovascular risk factor?
Fernando Margulis1, Roberto Sabbatiello1, Veronica Golglid1, Carlos Cuevas1, Claudia Castro2, Veronica Aguirrezabala2, Miriam Martinez3, Ruben Schiavelli1.
1Division de Nefrologia y Trasplante Renal, Hospital General de Agudos Dr. Cosme Argerich, Ciudad Autonoma de Bs As, Argentina; 2Laboratorio Central, Hospital General de Agudos Dr. Cosme Argerich, Ciudad Autonoma de Bs As, Argentina; 3Division de Alimentacion, Hospital General de Agudos Dr. Cosme Argerich, Ciudad Autonoma de Bs As, Argentina
Introduction: Kidney transplantation with living donor (LKD) is associated with longer graft and patient survival compared with deceased donor organs. Until recently, it was believed that the long-term risk of end-stage renal disease (ESRD), cardiovascular events (CVE) or death in LKD is similar to or even smaller than the general population. Normotensive salt-sensitive (Ss) subjects over 25 years old have a mortality similar to that of hypertensive subjects, while salt-resistant (Sr) normotensive subjects have a longer survival.
Objective: To compare, in healthy subjects that we have studied to be a LKD, the levels of 24 hour mean ambulatory blood pressure monitoring (24 hs mABPM), kidney function and left ventricular mass index (LVMI) between Ss and Sr, before and a year after donation.
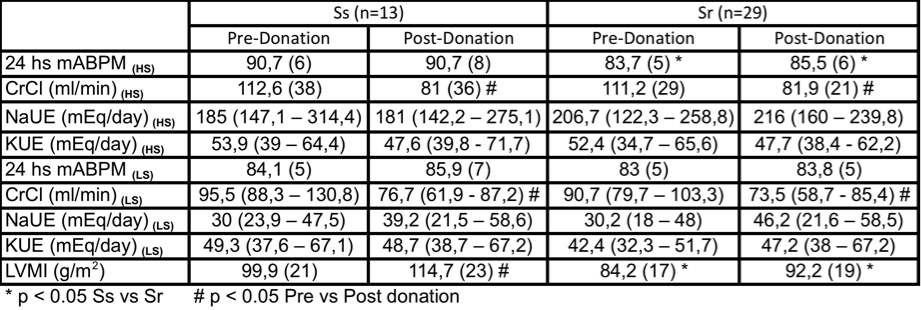
Methods: Data from 42 LKD were included. There were 34 (82%) women, with a mean age of 49 (11) years (range 26 to 66 years). None had a history of kidney disease, diabetes, CVE or hypertension. The subjects were placed on a high-salt diet containing 250 mmol Na for 7 days and on a low-salt diet containing 30 mmol Na during the following 7 days. Compliance with the diet was assessed twice a week by measurement of 24-hour urinary Na excretion (NaUE). On the last day of both the high and low-salt periods, 24-hour ABPM was performed with an automated, noninvasive device. Salt-sensitivity (SS) was defined by a significant decrease (P<0.05) of 24 hs mABPM from high to low salt intake. Trans-thoracic m-mode echocardiograms were performed on the last day of the first period. LV mass was calculated according to the Penn convention and corrected for body surface area to produce the LVMI. Data with normal and nonparametric distribution were expressed as mean and standard deviation (SD) or median and interquartile range (ICR), Student t test and Wilcoxon test were used respectively, P values < 0.05 were considered to be statistically significant.
Results: SS was found in 13 of the 42 living kidney donors (31%). The Ss group were older than Sr 53 (10) vs 47 (10) years, but it was not statistically significant (p=0.08). Pre-donation, with high-salt diet the 24 hs mABPM was significantly greater in Ss than in Sr, without any differences in creatinine clearence (CrCl), 24 hs NaUE and 24 hs potassium urinary (KUE) excretion. On the other hand with low-salt diet we did not find any significant differences in 24 hs mABPM, CrCl, NaUE and KUE between groups. LVMI was significantly greater in Ss than in Sr donors. One year after donation we found the same statistically differences in 24 hs mABPM with high-salt diet and no differences with the low-salt diet. Again LVMI was significantly greater in Ss than in Sr donors. The increase of LVMI after donation was significant only in Ss donors (23,2 vs 4,5 g/m2).
Conclusion: Ss healthy LKD showed a greater LVMI than Sr ones and a greater increment one year after donation. The study of SS could be included to make kidney transplantation with living donor organs safer.

right-click to download
