Mixed minimally invasive surgical modalities in living donor kidney transplant: outcomes and surgical complications
Michael McCabe1, M. Katherine Dokus2, Kate Helbig2, Erika Venniro2, Karen Pineda-Solis2, Amit Nair2, Jeremy Taylor3, Mark Orloff2, Roberto Hernandez-Alejandro2, Guan Wu4, Randeep Kashyap2.
1School of Medicine and Dentistry, University of Rochester, Rochester, NY, United States; 2Department of Surgery, Solid Organ Transplant, University of Rochester Medical Center, Rochester, NY, United States; 3Department of Medicine - Nephrology, University of Rochester Medical Center, Rochester, NY, United States; 4Department of Urology, University of Rochester Medical Center, Rochester, NY, United States
Introduction: The approaches through which living donor kidney transplant may be performed has greatly expanded, with both laparoscopic and robotic donor nephrectomy shown to be safe and feasible techniques. Moreover, robotic assisted kidney transplant continues to gain popularity. However, variance in patient anatomy and other factors means some living donor-recipient pairs may have different surgical approaches. This study aimed to address the lack of data on this topic by comparing postoperative renal function and surgical complications in living donor-recipient pairs with mixed surgical modalities.
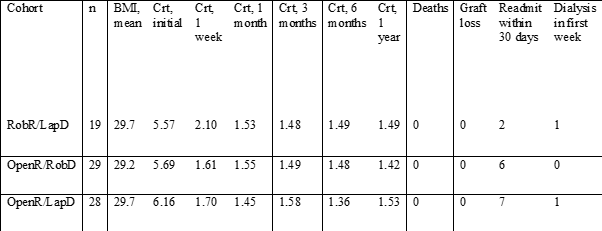
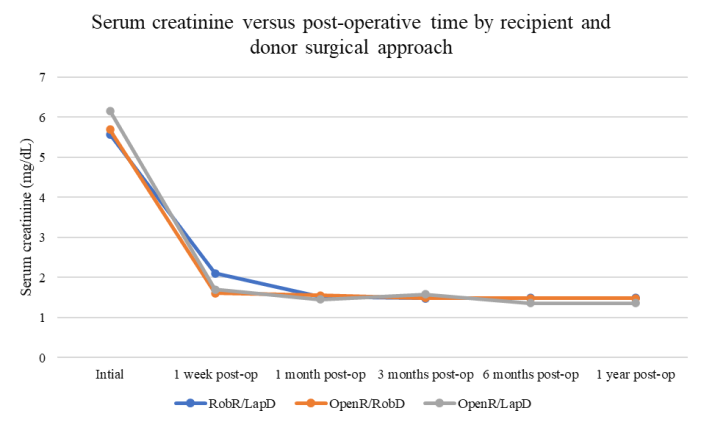
Methods: Institutional records of living donor kidney transplants from 2019 through 2022 were reviewed. Patients were included if their donor surgery was completed through a minimally invasive approach (either laparoscopic or robotic). Patients were classified into three groups based on recipient and donor surgery type: robotic recipient/laparoscopic donor (RobR/LapD); open recipient/robotic donor (OpenR/RobD); open recipient/laparoscopic donor (OpenR/LapD). Records were reviewed for serum creatinine preoperatively and at 1 week, 1 month, 3 months, 6 months and 1 year post-operatively. Patient demographics as well as number of deaths, graft losses, and readmissions within 30 days after surgery were likewise collected. Descriptive statistics were performed; continuous variables were compared with ANOVA; categorical variables were compared with Chi-squared.
Results: There were 290 renal transplants performed in the selected years. Of these, 76 patients met criteria for inclusion: 46 male and 30 female. The mean age was 54 years (24 – 78); mean BMI was 29.6 (17.7 – 41.6). There was no significant age, sex, or BMI difference between the cohorts (F=0.085, p=0.91; χ2=2.81, p=0.245). There was no significant difference between 1 week, 1 month, 3-month, 6-month or 1 year follow up creatinine levels between the groups (F=0.128, p=0.88). No deaths or incidences of graft loss occurred. One patient in the RobR/LapD group and one patient in the OpenR/LapD group required dialysis within the first week after transplant. There was no significant difference between rates of readmission within 30 days (χ2=1.52, p=0.467).
Conclusions: This study provides evidence that postoperative renal function and readmission rates does not vary significantly depending on donor and recipient surgical approach for living donor kidney transplant. Notably, robotic recipients had equivocal outcomes to the open recipient groups in all measured variables. Further work should study larger cohorts and delineate potential advantages of minimally invasive approaches such as rates of surgical site infections and wound complications.

right-click to download
