Pregnancy-induced sensitization in female transplant candidates: HLA-specific memory B cells and paternal HLA epitope mismatch
Sara Sanz-Ureña1, Laura Llinàs-Mallol1, Jorge Eguía1, María José Pérez1, Gonca E. Karahan2, Sebastiaan Heidt2, Carla Burballa1, Julio Pascual1, Dolores Redondo-Pachón1, Marta Crespo1.
1Nephropathies Research Group - Nephrology Department, IMIM - Hospital del Mar, Barcelona, Spain; 2Transplant Immunology Research Group, Dept. Immunology, Leiden University Medical Center, Leiden, Netherlands
Background: Access to kidney transplantation (KT) may be limited by HLA antibodies (HLA-Ab) induced by sensitizing events. Pregnancy is a frequent sensitizing event in female candidates, through which they are exposed to foreign paternal HLA antigens. Consequently, they can generate specific HLA-Ab and memory B cells (mBc), which can be re-stimulated upon antigen reencounter after KT. We aimed to study the existence of mBc able to produce specific HLA-Ab against paternal antigens in female KT candidates sensitised by previous pregnancies, to compare them with HLA-Ab found in their serum and to analyse these HLA-Ab in the context of the molecular HLA mismatch between mother and father.
Methods: We selected 8 HLA sensitised women awaiting KT with at least one successful pregnancy from a single partner, detectable serum HLA-Ab (MFI≥1000) and available paternal DNA for full HLA typing. All women and their partners were typed by next-generation sequencing for HLA–A, B, C, DRB1, DRB3/4/5, DQB1/A1, DPB1. To study mBc, we used peripheral blood mononuclear cells cryopreserved before KT and cultured them with a polyclonal stimulation cocktail consisting of a toll-like receptor agonist and an interleukin for ten days. We examined concentrated culture supernatants (SN) derived from activated mBc, purified IgG and identified HLA-Abs using single antigen beads on Luminex®. Then, we compared the HLA-Ab profiles of SN and serum. We also studied the paternal molecular HLA mismatch with HLAMatchmaker® software.
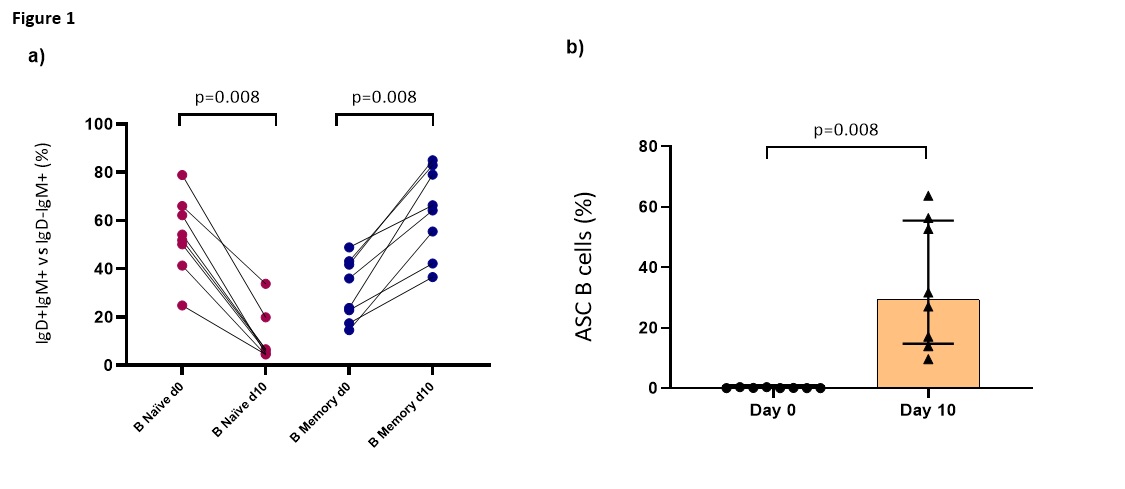
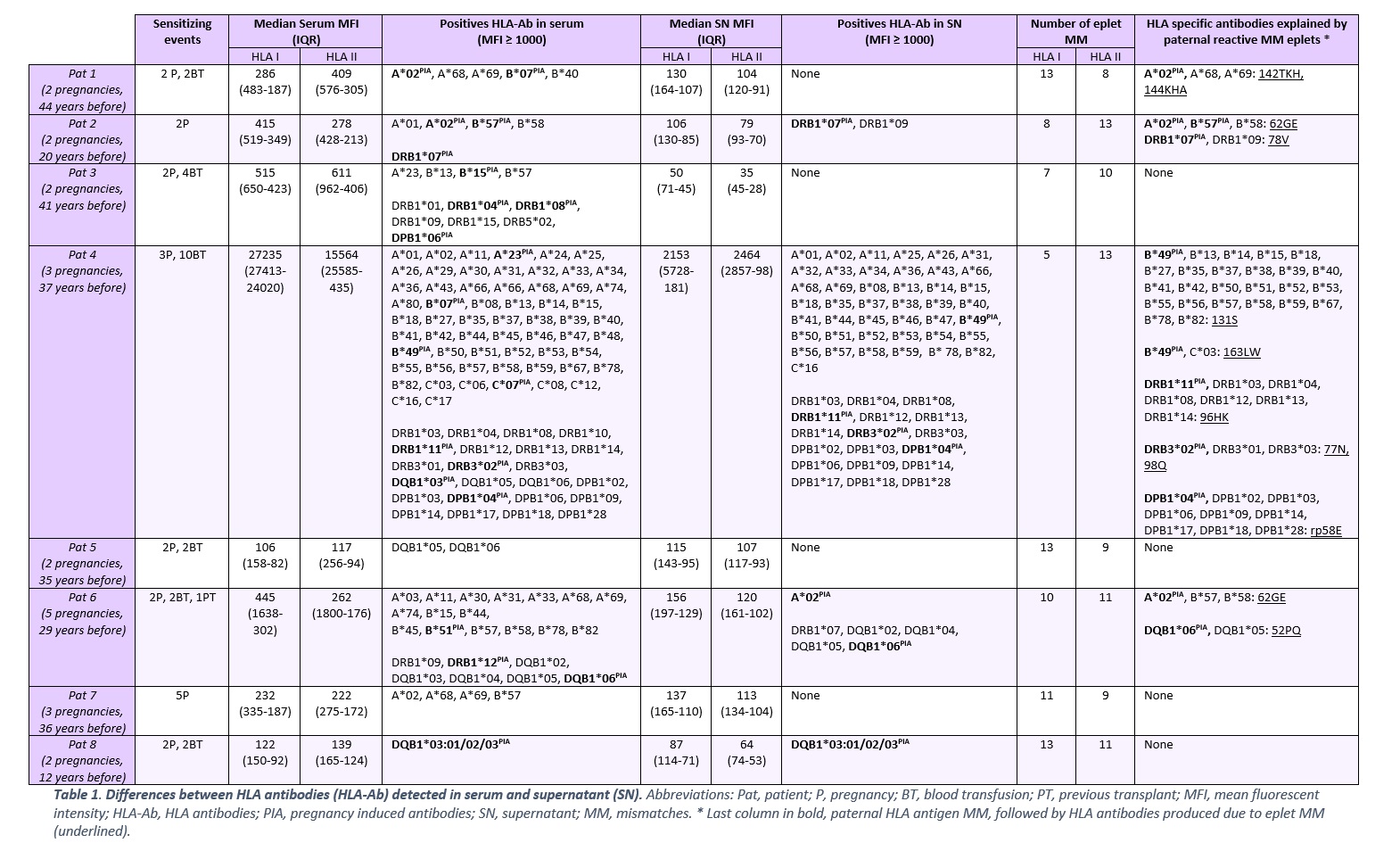
Results: After 10-day polyclonal stimulation, mBc increased from 29.9% (day 0) to 65.3% (day- 10), and antibody-secreting cells (ASC) from 0.1% (day-0) to 29.4% (day-10) (Figure 1). SAB analysis revealed 211 HLA-Abs in serum and 116 in SN: 98/211 (46,5%) HLA-Ab were serum-exclusive (79,6% class I and 20,4% class II) and only 3/116 (2,3%) HLA-Ab were SN-exclusive, all class II. Finally, we found 113/327 (34,6%) HLA-Ab shared by serum and SN: 65/113 (57,5%) class I and 48/113 (42,5%) class II.
Pregnancy-Induced Antibodies (PIA) were present in serum in 6/8 women (21 HLA-Abs: 10 class I, 11 class II) and in 4/8 women in SN (8 HLA-Abs: 2 class I, 6 class II). The HLAMatchmaker analysis showed that those specific HLA-ab were reactive against incompatible paternal epitopes: in 3/6 women for class I & 3/6 women for class II in serum; in 2/4 women for class I & 3/4 women for class II in SN (Table 1).
Conclusion: We describe the study of the memory B cell compartment and the HLA-Abs produced with Luminex technology in KT female candidates with previous pregnancies. We found that the HLA-Abs secreted by memory B cells followed a restricted pattern compared with serum HLA-Ab. The study of paternal HLA molecular mismatch explains many of these HLA-Abs decades after pregnancies. The entire value of this tool for risk stratification in HLA-sensitised patients awaiting TK is currently a matter of study.

right-click to download
