Clinical outcomes of simultaneous heart liver kidney transplant recipients, single center experience
Juhi Bhargava1, Sambhavi Krishnamoorthy1, Yousuf Kyeso1.
1Transplant Nephrology Medicine, University of Chicago, Chicago, IL, United States
Introduction: Multiorgan dysfunction involving the kidneys is not uncommon in patients with end stage heart and liver disease. Simultaneous heart-liver-kidney transplants (HLK) are less commonly performed than simultaneous heart-kidney or liver-kidney transplants due to the complex nature of the surgery and challenges with patient selection. 19 HLK were performed in the US from 2008 to 2020, out of which 8 were performed at our center. Given the limited availability of organs for transplant and the lack of standardized qualifying criteria for these patients, it is imperative to understand the factors involved in better outcomes, to optimize utilization of scarce resources.
Method: We performed a retrospective review of all HLK recipients at the University of Chicago medical center between 2008-2020 using Epic EMR. We evaluated their renal outcomes, infection rates, number of hospitalizations, and mortality over a 12-month period post transplantation.
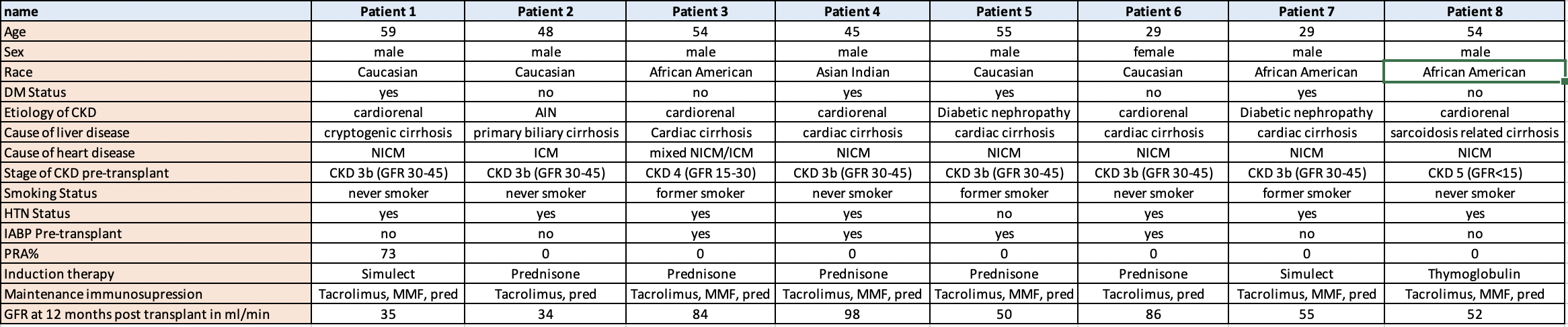
Results: Baseline characteristics are summarized in the table 1. 4(50%) were between the ages of 50-64, 2(25%) were between the ages of 35-49, and 2(25%) were between the age of 18-34. Four (50%) were Caucasians, 3(37.5%) were African Americans, and 1(12.5%) was Asian Indian. 6 (75%) had pre-transplant GFR between 30-40 ml/min, 1(12.5%) had GFR between 15-30 ml/min, and 1(12.5%) had GFR <15 ml/min. The etiology of CKD was as follows, 5(62.5%) were cardiorenal, 2(25%) were diabetic, 1(12.5%) was acute interstitial nephritis. All had Kidney Donor Profile Index (KDPI) below 20%. All had GFR above 50 ml/min at 3 months post-transplant, out of which 5 (62.5%) had GFR above 60 ml/min. At 6 months and 1 year, 3 (37.5%) had GFR above 60 ml/min, 3 (37.5%) were between 45-60 ml/min, and 2 (25%) had GFR between 30-45 ml/min. Only 1 patient developed delayed graft function requiring 2 sessions of dialysis post-transplant. All 8 were alive with intact kidney allograft function at 12 months after transplant. Only 2(25%) required a hospitalization within the 1st year of transplant for infection related reason. 2(25%) developed BK viremia and 2(25%) developed CMV viremia.
Conclusion: Our experience suggests that with careful selection of patients, simultaneous HLK can lead to successful patient outcomes at one year post transplantation. Longer follow up of these patients is needed to define long term allograft and patient survival which will help to standardize selection and allocation criteria of this subset of patients.

right-click to download
