Impact of HLA-A,B DR and DQ on living kidney transplant outcomes in the tacrolimus/MMF era: an artificial intelligence approach
Hatem Ali1, Mahmoud Mohammed3, Bernard Burke4, David Briggs2, Nithya Krishnan1.
1Renal department, University Hospitals of Coventry and Warwickshire, Coventry, United Kingdom; 2NHSBT, Birmingham, United Kingdom; 3University Hospitals of Mississippi, Mississippi, United States; 4Research Centre for Sport, Exercise and Life Sciences, Coventry University, Coventry, United Kingdom
Introduction: One of the biological barriers that can impact outcomes among Living donor kidney transplantation is HLA mismatch. The aim of our study is to assess the effect of HLA mismatches on acute rejection rates and graft survival in the Tacrolimus era. Moreover, to assess factors affecting survival.
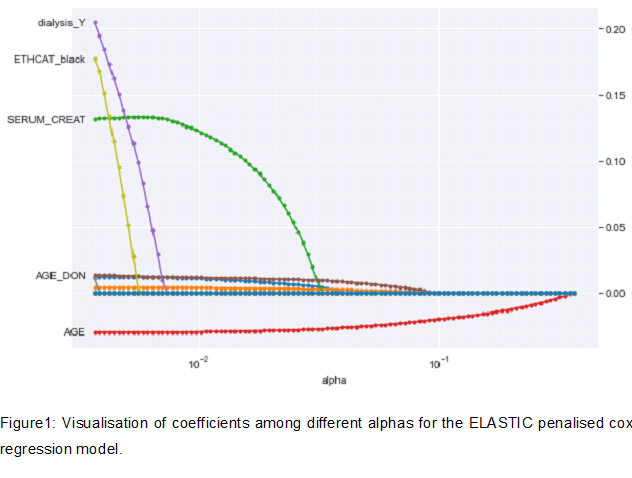
Methodology: All Living donor kidney transplant patients registered in UNOS database between 01/01/2005 and 01/12/2019 were retrospectively reviewed. Inclusion criteria: Living donor transplant recipients that were discharged on Tacrolimus/Mycophenolate Mofetil. Exclusion criteria: multiple organ transplants, previous kidney transplants, recipient age<18 years old, deceased donor transplants, missing data about induction therapy, missing HLA mismatch or ABO incompatible transplant. We used double-selection lasso (least absolute shrinkage and selection operator) logistic regression model to assess for acute rejection rates at one-year post-transplant. Variables of interest were HLA-A,B,DR and DQ mismatch. Variables Lasso selected from were: recipient characteristics (age, sex, BMI, ethnicity, diabetes, recipient/donor CMV status, pre-transplant dialysis), donor characteristics (age,ethnicity, diabetes and hypertension) and transplant characteristics (induction therapy, steroid intake, cold ischemia time, delayed graft function, PRA). Acute rejection was defined as biopsy proven or clinically suspected rejection. For survival analysis, we fit a penalised Cox model after choosing best alpha. Cross-validated grid-search was used to evaluate the best alpha. The variables included in the penalised cox model donor, recipient and transplant factors plus HLA mismatches.
Results: 28,736 patients were included in our study. Worse acute rejection rates at one-year post-transplant were noted with incremental increase in HLA-DQ (Two HLA-DQ: OR=1.29, P<0.01, 95%CI:1.08-1.54; One HLA DQ:OR=1.22,P=0.01, 95%CI:1.05-1.44), HLA-DR mismatches (Two HLA-DR: OR=1.85, P<0.01, 95%CI:1.48-2.31; One HLA-DR: OR=1.51,p<0.01, 95%CI:1.23-1.85) ,HLA-B mismatches( Two HLA-B OR=1.33, P=0.01,95%CI:1.05-1.69; One HLA-B mismatch: OR=1.21,P=0.09) and HLA-A mismatch (OR:1.19, P<0.01). In the penalized cox regression model, None of the HLA types (A,B,DR or DQ) were associated with worse graft survival (P>0.05 for every type). The factors that were associated with worse outcomes are: Recipient black ethnicity (HR 1.2, P<0.01, 95%CI:1.10-1.31); delayed graft function (HR=1.54, p<0.01, 95%CI:1.31-1.81), pre-transplant dialysis (HR=1.19,P<0.01, 95%CI:1.12-1.26) and donor Black ethnicity(HR=1.21, P<0.01, 95%CI:1.10-1.33).
Conclusion: HLA-DQ, DR,B and A mismatches play a vital role in the occurrence of acute rejection among Living donor kidney transplant recipients. However, HLA mismatches have no significant effect on graft survival. Delayed graft function, pre-transplant dialysis recipient and donor black ethnicity, play an important role in determining graft survival.

right-click to download
