Why do not all living kidney donor candidates are accepted for donation? A pediatric center experience
Alfonso Navarro-González1, Monserrat Arreola-Gutiérrez1, Juan C Barrera-De León2, Ana B Calderón-Alvarado3, Mitzi R Becerra-Moscoso3, María J Ruiz-López3.
1Transplant - Urology and Nephrology Department, Hospital de Pediatría CMNO IMSS, Guadalajara, , Mexico; 2Research and Teaching Department , Hospital de Pediatría CMNO IMSS, Guadalajara, , Mexico; 3Pediatric Surgery Department, Hospital de Pediatría CMNO IMSS, Guadalajara, , Mexico
Introduction: Living donor kidney transplantation is the best type of renal replacement therapy for patients with end-stage renal disease, providing numerous clinical benefits when compared with prolonged dialysis or deceased donor kidney transplantation. These include longer patient and graft survival, decreased waiting period on the transplantation list and improved quality of life. Living kidney donors (LKDs) go through an extensive evaluation to ensure the safety before proceeding for donation, and many potential LKDs are declined because of different reasons. The aim of this study was to define the reasons for declining potential LKDs referred to our center.
Methods: We retrospectively analyzed clinical data of all potential LKDs evaluated between January 2001 and December 2021, at our institution CMNO, Pediatric Hospital. Data were obtained by review of an electronic database. Data for quantitative variables were presented as mean, standard deviation and range, and categorical variables as frequencies and percentages.
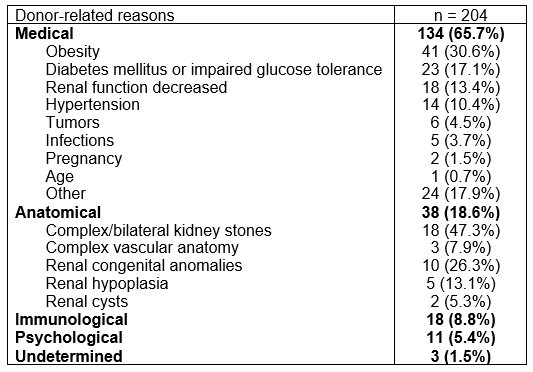
Results: A total of 1332 potential LKDs were evaluated, 796 (59.7%) successfully donated, 20 (1.5%) has a complete evaluation, accepted for donation and in waiting list for intervention, 56 (4.2%) continues in evaluation process, 200 (15%) were discharge from the program due to administrative aspects, death (donor or receptor) or cadaveric renal transplantation in order of frequency, 56 (4.2%) withdraw by personal choice at variable time points during the evaluation process, and 204 (15.3%) were rejected for donation. Donor-related reasons included medical contraindications (n=134, 65.7%), anatomical contraindications (n=38, 18.6%), immunological barriers (n=18, 8.8%), and psychological reasons (n=11, 5.4%).
Conclusions: Despite the large number of potential LKDs a significant proportion do not proceed for donation at some point during the evaluation process, in our description, it represents 40.3%, a total of 536 patients that keep waiting for a kidney transplant. Most of the reasons are consequence of candidate’s medical conditions, standing out the prevalence in our population of unnoticed chronic diseases (obesity, diabetes mellitus, impaired glucose tolerance, hypertension) and its impact on kidney function. Since the deceased donor pool is limited and provides fewer benefits, modifying accepting criteria such as accepting potential LKDs with mild obesity or well-controlled hypertension might be needed. These numbers highlight the need for increased public awareness of living donation, more careful but inclusive screening, targeted educational programs, and ongoing support for potential LKDs.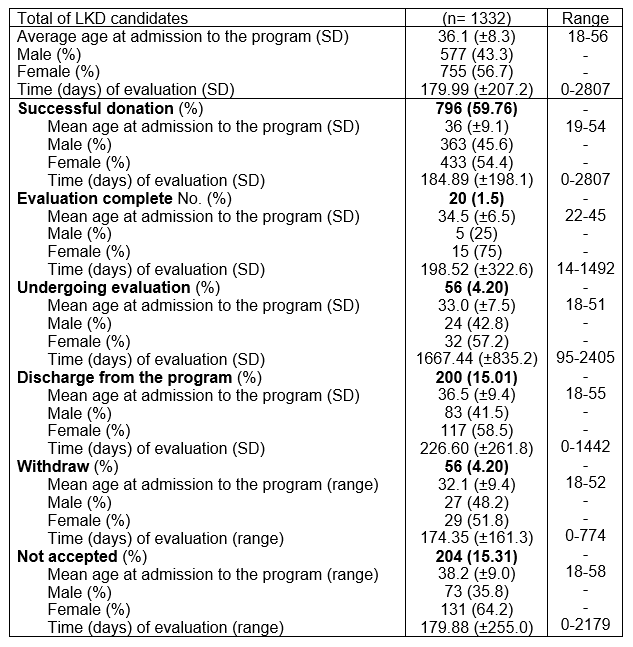

right-click to download
