Parenteral nutrition free survival in pediatric patients with short bowel syndrome: transplantation vs. serial transverse enteroplasty (STEP), a paired matched case-control study
Gimena Galdeano1, Carolina Rumbo1, María Inés Martínez1, Gabriel Gondolesi1.
1Hepato-bilio-pancreatic surgery, Fundación Favaloro, Ciudad Autónoma de Buenos Aires, Argentina
Introduction: Intestinal failure (IF) is a reduction of the intestinal function below the minimum necessary for the absorption of macronutrients, water and electrolytes to sustain life growth and in children, making parenteral nutrition (PN) the primary therapeutic approach. The causes of intestinal failure can be anatomic or functional, being short bowel syndrome (SBS) the most frequent. Currently a comprehensive multidisciplinary management provides different alternatives like medical rehabilitation, surgical rehabilitation or intestinal transplantation (ITX) in order to recover intestinal sufficiency. The indications of the different approaches have been modified over the course of the years, and comparison assessments are lacking.
Objective: To compare the time necessary to achieve PN independency, nutritional outcome, and long-term survival of pediatric patients with IF SBS treated with intestinal transplant (ITX) or STEP, at our center.
Materials and methods: Observational, analytical, matched case-control and retrospective study, of a group of patients treated from 2006 to 2022 at our unit. The data was collected through review of the patients’ medical records.
Results: A sample of 22 pediatric patients with SBS was selected; two of them were excluded to lack of follow-up; therefore 20 patients met all the criteria and are analyzed. The mean age of the ITx patients was 12.32 ± 4.8 (p=NS), of which 60% were male; while in the STEP group, mean age was 9.24 ± 2.7; 90% were male. Primary diagnoses are shown in table 1.
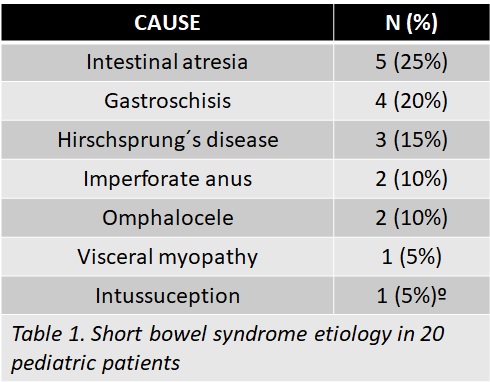
ITX restored the intestinal length to a 100%, whilst STEP allowed for a benefit of 53.6 +/- 34.98 cm. ITX patients required less time to achieve freedom from PN survival compared to STEP (p=0.001, Figure 1a), 80% of them sustained it throughout the first year; in the STEP group, only 30% of the patients achieved PN independency during that time. Furthermore, 5 years after the procedures, no significant differences were found regarding freedom from PN survival between groups (p=NS, Figure 1b). ITX patients gained a significant amount of weight after 6 months (p˂0.0001); while the same effect was observed in STEP patients after 12 months (p=0.004). At 5 years, PN free survivors both in the ITX group and the STEP group were able to sustain weight, in fact a significant difference was obtained comparing with baseline (p<0.0001) and the first year (p=0.0005).
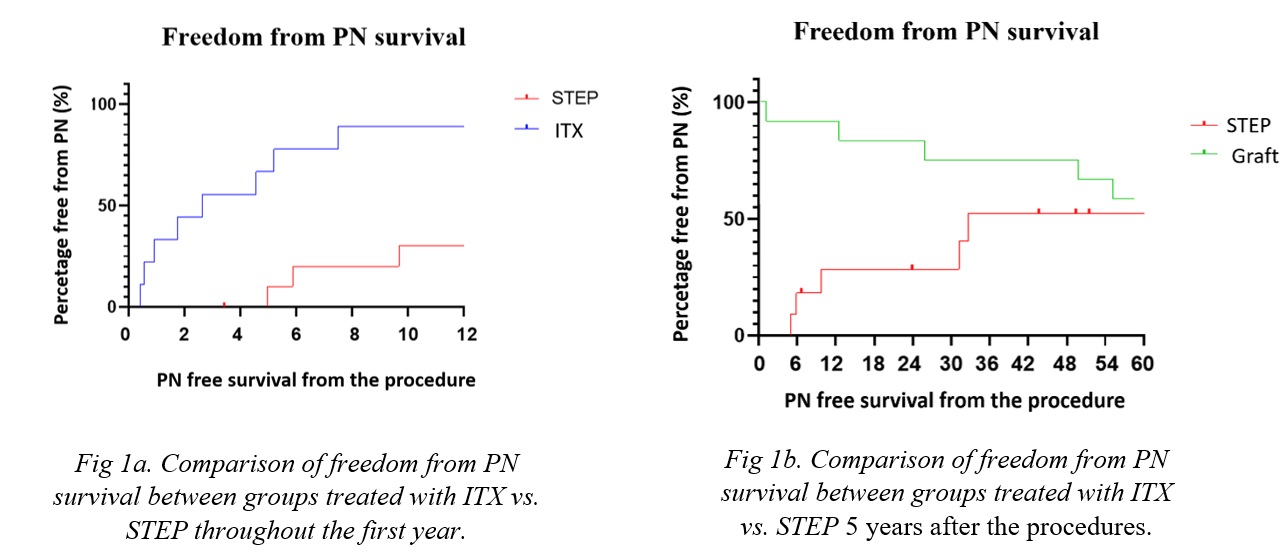
No significant differences were found between those treated with STEP and ITX patients (p=NS) when analyzing the 5-year actuarial survival.
Conclusion: Although with different indications, ITX and STEP allowed a similar percentage of patients achieving 5 years survival free from PN. The initial higher slope observed in the ITX group, decreases in the long term due to intestinal graft loss. STEP required longer time achieve PN independency. Future studies would allow analyzing the long-term impact of both procedures.

right-click to download
