Miami protocol for liver deceased donors after circulatory death: increased 1-year overall survival for selected patients
Phillipe Abreu1, Vighnesh Venkatasamy1, Juliano Riella1, Giselle Guerra1, Rafael Miyashiro1, Alfred Joseph Tector1, Akin Tekin1, Gennaro Selvaggi1, Rodrigo Vianna1.
1Department of Transplantation Surgery, Jackson Memorial Hospital, University of Miami, Miami Transplant Institute, Miami, FL, United States
Background: The use of deceased donors after circulatory death (DCD) for liver transplantation (LT) is still underutilized. It provides an acceptable solution to increase the organ donor pool without affecting outcomes. We analyzed data of DCD donors for LT in order to identify risk factors for graft and patient survival.
Methods: This was a retrospective cohort study using data reviewed by screening SRTR/UNOS of patients that underwent liver transplantation with DCD donor at the University of Miami, Jackson Memorial Hospital in Miami, FL from 2017 to 2019. Different surrogates were analyzed, including donor, recipient, procurement and transplant operation characteristics. The primary outcome was patient and graft survival. Continuous variables were analyzed using a 2-sided student t-test. Categorical variables were presented as frequencies and proportion and compared using chi-squared or Fisher’s exact test as appropriate. Univariable Cox proportional hazards models were fit in order to assess the impact of individual covariables on the instantaneous rate of events, with time-to-event analysis also being ascertained through Kaplan-Meier estimates.
Results: 54 cases were analyzed with a median MELD score of 18.5. Alcoholic cirrhosis was the most prevalent etiology for liver disease.
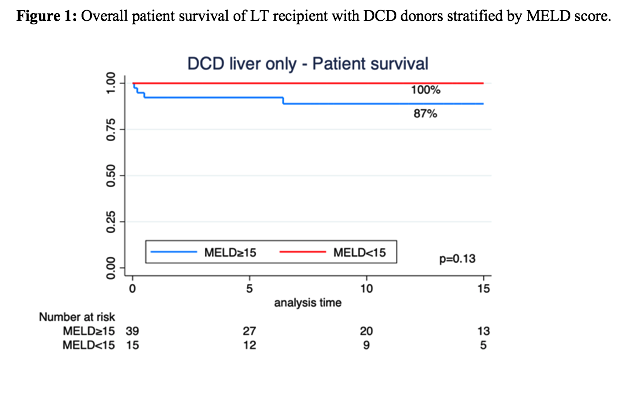
There was 1 case with intra-hepatic biliary stricture, and 7 patients with anastomotic strictures that required stenting. The 1-year survival rate following liver transplant using DCD donors was 90.7%. The total cold ischemic time (CIT) (HR 1.9, 95% CI 1.1-3.2) and diagnosis of rejection (HR 9, 95% CI 1.1-78.8) were statistically significant affecting graft failure. Estimated blood loss (EBL) with HR of 1.1 (95% CI 1.1-1.2) was found to be statistically impacting survival rate.
Conclusion: DCD donors are excellent options to increase the availability of organs for patients waiting for a LT. CIT and EBL are the main predictors of poor outcomes and thus should be carefully taken into account when matching organs to recipients.

right-click to download
