Update on the long-term follow-up of kidney donors from a single center in Argentina (hospital italiano de Buenos Aires)
Carlos Schreck1, Cesar A Mombelli1, Daiana M Zapata1, Henrry M Darquea Sanchez1, Nora C Imperiali1, Susana K Villamil Cortez1, Silvia R Groppa1, Guillermo J Rosa Diez1, Maria C Giordani1.
1Nephrology, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina
Introduction: Living kidney donors are selected upon kidney and overall health. Only those with a low/minimal risk of developing progressive CKD are accepted. Clinical studies have shown that the risk of developing end-stage renal disease (ESRD) in donors is similar to that in the general population Nonetheless, long-term follow-up is of utmost importance to ensure they are properly monitored and receive timely and adequate medical care. We present our updated data on the long term follow-up of our population over the last 22 years.
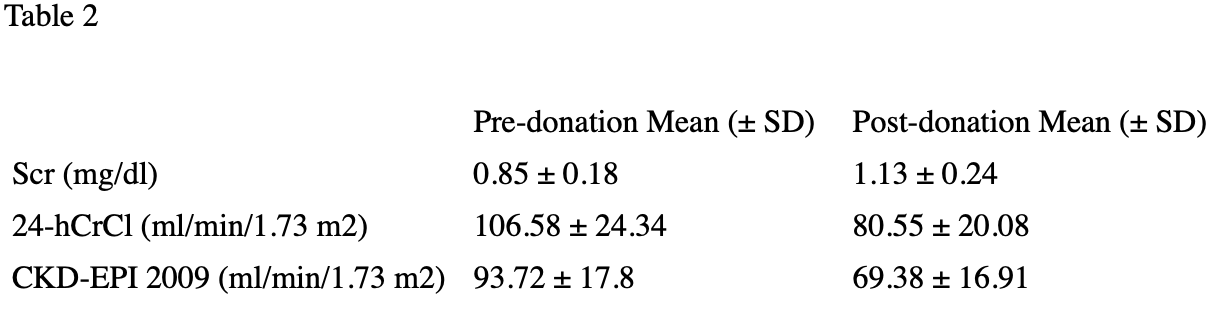
Methods: Our data includes laboratory and clinical data on 197 patients who were donors between 2000-2022. The variables analyzed were: 1) GFR as Scr, eGFR (CKD-EPI 2009) and 24-h CrCl. 2) Proteinuria as 24-h microalbuminuria. 3) Hypertension. 4) Body Mass Index. 5) Renal Functional Reserve (RFR). We correlated post-donation GFR with expected GFR (adjusted to age and single kidney). Pre-donation RFR was correlated with post-donation GFR. Univariate analysis was used to compare pre and post-donation variables.
Results: Pre-donation demographic and clinical/lab data are shown in Table 1. As expected, GFR was significantly lower after donation (table 2). Post-donation GFR was significantly lower from expected GFR (80.55 vs 88.64 ml/min/1.73 m²,, p < 0.0001). However, the CKD stage (KDIGO 2) was not different in either scenario ( measured vs expected). 2 donors (1%) with microalbuminuria slightly higher than 27 mg/d were accepted for donation. After donation, the mean value for microalbuminuria was not different from pre-donation (p=0.22), and only 2 previously normoalbuminuric patients increased microalbuminuria above 27mg/d. Pre-donation hypertensives amount to 10,2% of our population. Out of the 177 normotensive donors, only 17 developed hypertension after donation (9.6%). Donors with a RFR > 45 % (median of our population) had a tendency towards a higher GFR assessed by 24h-CrCl (72.94 ± 16.89 vs 66.96 ± 17.31 ml/min/1.73 m2) which did not reach statistical significance ( p = 0.119). BMI was not significantly different after donation ( 27.5 ± 8.2 vs 26.84 ± 5.3 kg/m², p = 0.35).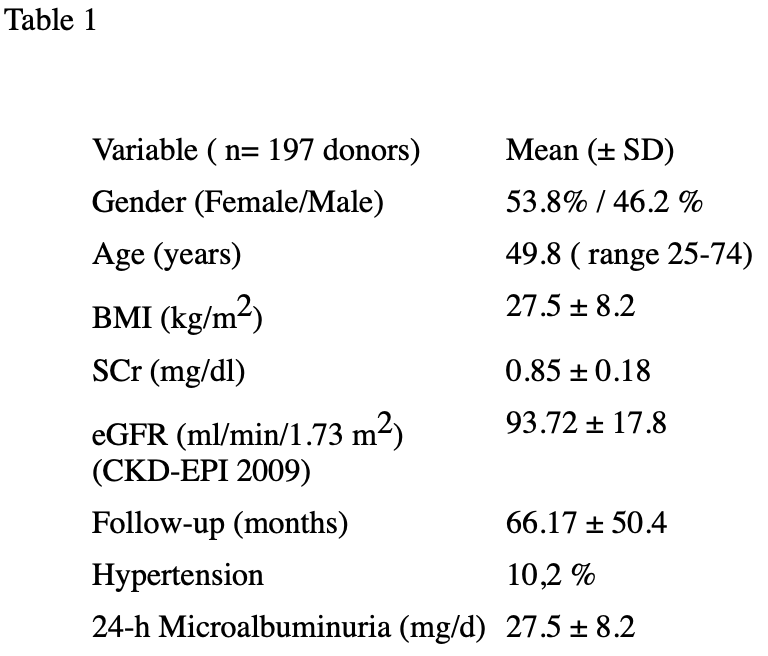
Conclusion: In our population, renal outcome was similar to that of healthy individuals after uninephrectomy. GFR was slightly lower than expected after uninephrectomy. However, it is unclear whether this difference is clinically significant.

right-click to download
