Renal failure in patients bridged to lung transplant with ECMO: risk factors and outcomes
Erin Isaza1, Marek Brzezinski2, Steven Hays3, Jonathan P Singer3, Jasleen Kukreja4.
1School of Medicine, University of California, San Francisco, San Francisco, CA, United States; 2Department of Anesthesia, University of California, San Francisco, San Francisco, CA, United States; 3Department of Medicine, University of California, San Francisco, San Francisco, CA, United States; 4Department of Surgery, University of California, San Francisco, San Francisco, CA, United States
Introduction: Extracorporeal membrane oxygenation (ECMO) is a well-established intervention as a bridge to lung transplantation (BTT) in critically ill patients with excellent outcomes. However, some patients deteriorate despite ECMO support, developing multiorgan failure including acute kidney injury (AKI), which often requires continuous renal replacement therapy (CRRT). While the majority of AKI-on-ECMO patients are no longer considered candidates for transplant, the outcomes of those patients who are transplanted despite AKI-on-ECMO are poorly understood. Therefore, this study examined risk factors for development of AKI-on-ECMO prior to transplant as well as the long-term renal outcomes in patients successfully transplanted with AKI-on-ECMO.
Methods: We retrospectively identified 84 patients who were supported on ECMO with the intent to BTT at our institution between 2010-2020. Outcomes of those who developed AKI-on-ECMO BTT were compared with those without AKI-on-ECMO BTT, as well as to those that developed AKI on ECMO but were not transplanted (failed BTT). χ2 test for independence for categorical variables and Student’s t-test for continuous variables were used. Renal function was examined for the first 3 years post-transplant in the patients transplanted with AKI to evaluate renal recovery.
Results: Forty-seven patients were successfully bridged to transplant, with 6 (12.8%) developing an AKI pre-transplant while on ECMO (2 of the 6 required CRRT pre-transplant). Patients with AKI had different lung pathologies (p=0.006), were more likely to be on central ECMO (p=0.002) compared to those without AKI-on-ECMO BTT and had longer post-transplant hospital stay (p=0.015). Of the 39 patients who failed BTT, 14 (35.9%) developed AKI. Compared to patients successfully transplanted with AKI, the failed BTT were shorter (p=0.045) and received more transfusions while on ECMO (p=0.035). All 6 patients with AKI-on-ECMO BTT required CRRT post-transplant for between 1 and 18 days; 4 patients were transitioned to intermittent hemodialysis (iHD) prior to discharge. Long-term, 2 patients had near-complete renal recovery within 2 months following transplant, 2 patients transitioned off iHD but without return of renal function to pre-transplant baseline, and the remaining 2 continued iHD. Five patients were alive 3 years post-transplant, with 1 death due to metastatic malignancy. At 3 years, mean peak post-transplant FEV1 %-predicted was 77.6 and no significant rejection events had occurred.
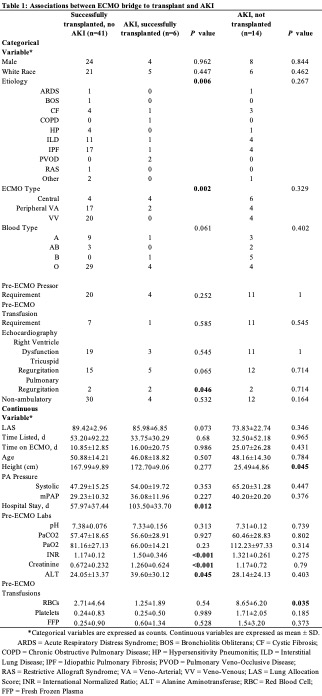
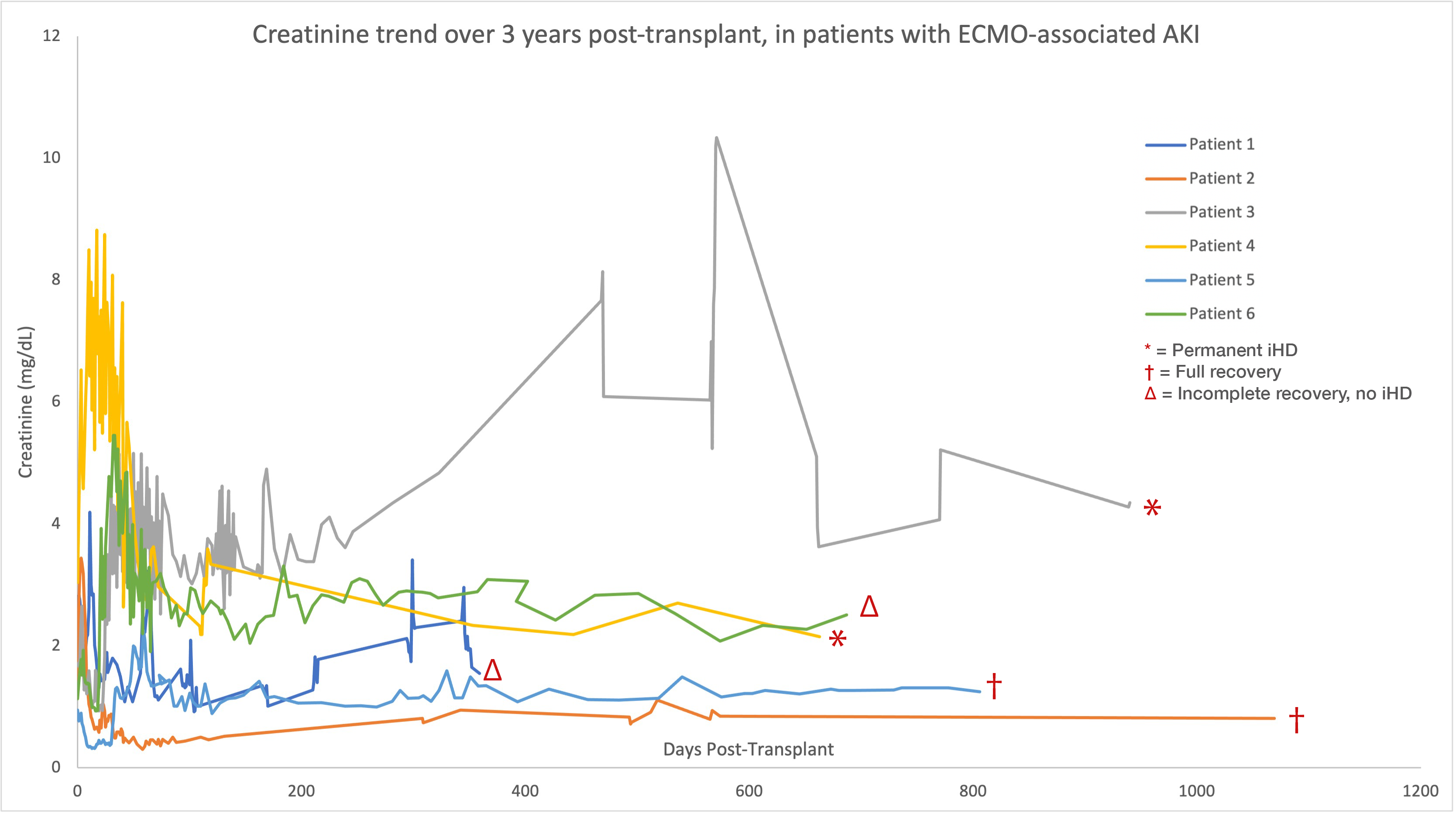
Conclusion: This study evaluated renal outcomes in patients who developed acute kidney injury while on ECMO as a bridge to lung transplantation. More than half of the patients did not require iHD within months, with the two youngest returning to their baseline creatinine. Our results suggest that AKI while on ECMO bridge may not represent an absolute contraindication to transplantation and in carefully selected patients can lead to optimal long-term outcomes.

right-click to download
